
Get FREE Weekly MRI Content

This step-by-step guide is for MRI students, radiographers and technologists who wish to improve their planning skills and master the cardiac viability MRI protocol.
This guide is Part 1 of a cardiac viability assessment. This first part will focus on:
In Part 2, cover with tissue characterization, where we determine which damaged parts of the myocardium can recover with treatment, and which are permanently scarred.
What you will learn in this Part 1:
To identify if damaged heart muscle can still heal, we must clearly distinguish between healthy and scarred myocardium. Strong SNR helps us differentiate bright scar tissues against dark healthy muscle.
Inversion Recovery is used for Black and Bright imaging to examine the heart’s structure and extra-cardiac findings. Cine imaging creates a live “movie” of the beating heart, which helps us assess its function.
| Artifacts | Solution – How to Avoid It |
|---|---|
| Motion | Use ECG-gating to synchronize image acquisition with the patient’s cardiac cycle and reduce heart motion. |
| Breathing | Instruct patients to hold their breath during imaging. Use breath-hold sequences when possible. |
| ECG mis-triggering | Use real-time cine imaging to minimize the impact of poor ECG signals or arrhythmias. |
| Flow | Align the phase encoding direction 90° to major vessels to reduce ghosting from blood flow. |
| Susceptibility | Increase the bandwidth to shorten readout time and reduce distortion from magnetic field variations. |
| Wrap-around | Use fold-over suppression or phase oversampling to prevent anatomy outside the FOV from overlapping. |
The heart is a vital organ that pumps blood throughout the body, delivering oxygen and nutrients to tissues. Heart disease remains the leading cause of death worldwide, so accurate heart imaging is key for diagnosis and treatment.
Cardiac viability MRI protocols are critical for evaluating myocardial damage caused by poor blood flow, often due to heart attacks or coronary artery disease (CAD).
These exams help us determine:
This information is crucial for deciding on treatments like revascularization or bypass surgery.

In MRI, we always face a trade-off between 3 key metrics:
Improving one of these metrics reduces the performance of the others. To decide what trade-offs to make, we must consider the needs of each clinical situation.
For viability MRIs:
Therefore, we typically 1) prioritize SNR, 2) keep high enough resolution to assess scar depth, and 3) optimize for scan time as needed based on patient ability.
This balance ensures we clearly see bright scar tissue against the dark, viable myocardium, which is the whole point of viability imaging.

The cardiac viability/MI MRI study can help us diagnose a wide range of heart conditions.
In this article, we focus specifically on conditions related to:
The table below lists some of the most common cardiac conditions related to these two aspects, and what pulse sequences reveal them:
| Common Cardiac Viability Conditions | Clearly Seen on Sequence | Why This Sequence? |
|---|---|---|
|
Extra-cardiac findings: • Pericardial effusions • Pleural effusions • Mediastinal masses |
Black Blood (IR-bSSFP) |
Nulls signal from blood while showing surrounding tissues. This makes it ideal for fluid collections and fat around the heart. Excellent for assessing the pericardium and thoracic anatomy. |
|
Chamber anatomy and abnormalities: • Thrombi • Cardiomyopathies • Ventricular hypertrophy |
Bright Blood (IR-TSE) |
Provides clear views of heart chambers. Bright blood enhances contrast with myocardium. Ideal for assessing wall thickness, cavity size, and structural defects. |
|
Functional abnormalities (LV): • Wall motion disorders • Systolic dysfunction (low EF) • Mitral regurgitation |
CINE SSFP (4ch, 2ch, 3ch, SAX) |
Captures a real-time “movie” of the heart’s motion through the cardiac cycle. Enables precise assessment of contraction, ejection fraction, and valve function. |
This step-by-step guide below will show you how to set up and perform a cardiac viability MRI protocol in practice, focusing specifically on the morphology and function aspects of viability.
We will perform the protocol in 3 parts:
Breath-holding is essential in cardiac MRI to avoid motion artifacts from the diaphragm and chest wall.
When a patient breathes during a scan, the heart and surrounding structures shift, which causes image blurring or ghosting.
To prevent this, we ask the patient to hold their breath at the end of exhale, which is the most stable phase of the breathing cycle.
🗣️ Example – How to Instruct the Patient:
“During the scan, I’ll sometimes ask you to breathe in, breathe out, and then hold your breath for about 10–12 seconds. Please stay as still as possible during this time.
We will repeat this practice several times during the scan. But don’t worry. You will have time to catch your breath between each breathhold.”
Let the patient practice once or twice before scanning. Watch their breathing pattern and give coaching if needed.
Cardiac MRI requires many repeated breath-holds, often 15 to 20 times, especially for cine and viability sequences.
If the patient has trouble with breath-holds (e.g., due to age, heart failure, or lung disease), use faster scan techniques or consider free-breathing alternatives with motion correction.
Lay the patient feet-first and supine (on their back) with the chest aligned at the scanner’s isocenter.
Using a feet-first position makes the scan feel less claustrophobic for the patient, which reduces the risk of motion artifacts.
Use a dedicated cardiac coil to ensure high-resolution imaging. This coil provides strong signal reception and full coverage of the heart.
✅ Correct Patient Positioning:

ECG-gating means we use the patient’s electrocardiogram (ECG) to capture each image at the same time point during each heartbeat.
Without gating, images may be acquired during different cardiac phases (points in time during a heartbeat), which leads to motion artifacts caused by heart movement.
To ECG-gate, you need to place three ECG electrodes on the patient’s chest, as shown in the image below:

These electrodes connect to the MRI-compatible ECG box, which tracks the heart’s electrical signal.
For this scan, we rely on a regular RR interval, meaning the patient has a normal sinus rhythm with consistent timing between beats.
If the patient has a heart condition, such as arrhythmia, they may have irregular timing between diastole and systole of the cardiac cycle. This variation can cause missed triggers or skipped beats, which result in artifacts or blurred images.
That’s why it’s essential to check the ECG signal before you begin.
The ECG trace is your guide for the entire scan.
If it’s unstable or disconnects during scanning, image quality may suffer.
Once the patient is in place, review your scanner’s hardware settings.
In this guide, we will use the following settings:
| Scanner Setting | Value | Why This Value |
|---|---|---|
| Magnetic field strength | 1.5 T | Enables high Signal-to-Noise Ratio, which gives superior image quality. (3 T gives even better signal and resolution, but also brings more artifacts and heat, so most scans use 1.5 T.) |
| Maximum gradient strength | 45 mT/m | Enables faster acquisitions while preserving high image quality. |
This hardware setup is widely used in clinical practice. It balances acquisition time, image quality, and patient comfort.
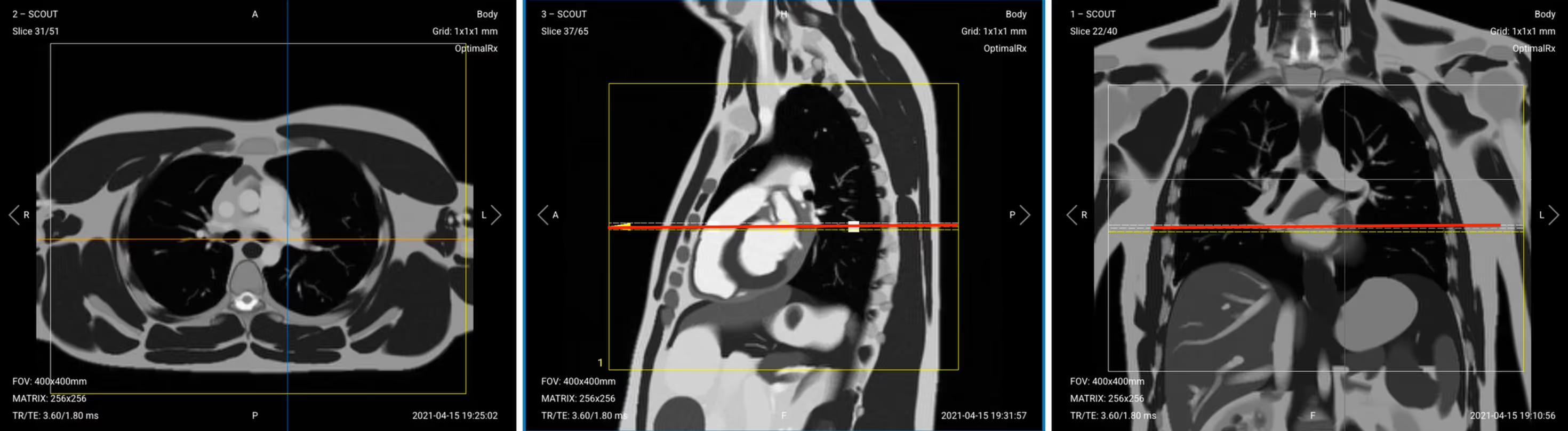
Before we can perform any MRI protocol, we must always capture initial localizer images of the patient. These images act as a guide for planning the detailed scans we will perform next.
We should always capture localizers in three planes:
Once acquired, upload the initial localizer images into the three viewports.
Then, scroll through each of the image stacks to locate a central slice that clearly shows the anatomy of the heart.
✅ Correct Setup of Localizer Images for Cardiac Viability MRI:

When all preparations are ready, we can start planning and acquiring the protocol sequences.
Let's go through the pulse sequences a standard cardiac viability MRI protocol includes, why we perform them, and how to set them up.
This article only focuses on sequences related to cardiac function and morphology.
For cardiac tissue characterization, we will run additional sequences such as perfusion and early/late gadolinium enhancement.
As you can see from this list above, we mainly use two types of sequences for this study:
Both types of sequences use ECG-gating to reduce motion artifacts and thus improve image quality.
In the sections below, we go through how to plan and set up each sequence.
The black blood sequence helps us see extra-cardiac structures, pericardial effusions, and fat infiltration.
✅ Correct Planning:
Planning Instructions:
Parameters for Black Blood (IR-bSSFP):
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 1.2–1.8 ms | Very short TE reduces susceptibility and banding artifacts in bSSFP and preserves blood nulling accuracy. |
| Repetition Time (TR) | 4.0–6.0 ms | Very short TR maintains the steady-state signal in bSSFP and supports rapid image acquisition. |
| Inversion Time (TI) | 800–900 ms | TI is timed to null the blood signal based on its T1 value at 1.5 T. |
| Field-of-View (FOV) | 380 × 320 mm | Covers the entire heart and mediastinum with acceptable resolution and minimizing aliasing. |
| Matrix | 192 × 256 | Medium matrix size balances spatial resolution, high SNR, and scan speed. Ideal for cardiac anatomy. |
| Foldover Direction (Phase) | Anterior-to-Posterior (AP) | Reduces motion artifacts from cardiac or respiratory motion, which typically occur in the superior-inferior direction. |
| Number of Slices | 25–40 | Ensures coverage from lung apices through the diaphragm to capture the full heart and mediastinum. |
| Slice Thickness | 6–8 mm | Thick enough for full myocardial coverage with good SNR; thinner slices may lose signal in bSSFP. |
| Slice Gap | 1–2 mm | Thin gaps reduce crosstalk and ensure full anatomical coverage without losing detail between slices. |
| NEX / Averages | 1–2 | One average keeps scan time short; a second average may improve SNR if motion is an issue. |
| Turbo Factor / ETL | N/A | Not applicable for bSSFP, which uses single-shot or segmented GRE readout rather than TSE. |
| Bandwidth | 192,000 Hz | High bandwidth shortens TE and reduces susceptibility and flow artifacts common in cardiac imaging. |
| Flip Angle | 50–70° | Optimized to enhance contrast between myocardium and suppressed blood signal while preserving SNR. |
| Fold-over Suppression | Yes | Prevents aliasing from arms, chest wall, or posterior structures entering the FOV. |
The bright blood sequence shows intra-cardiac anatomy and chamber dimensions.
✅ Correct Planning:
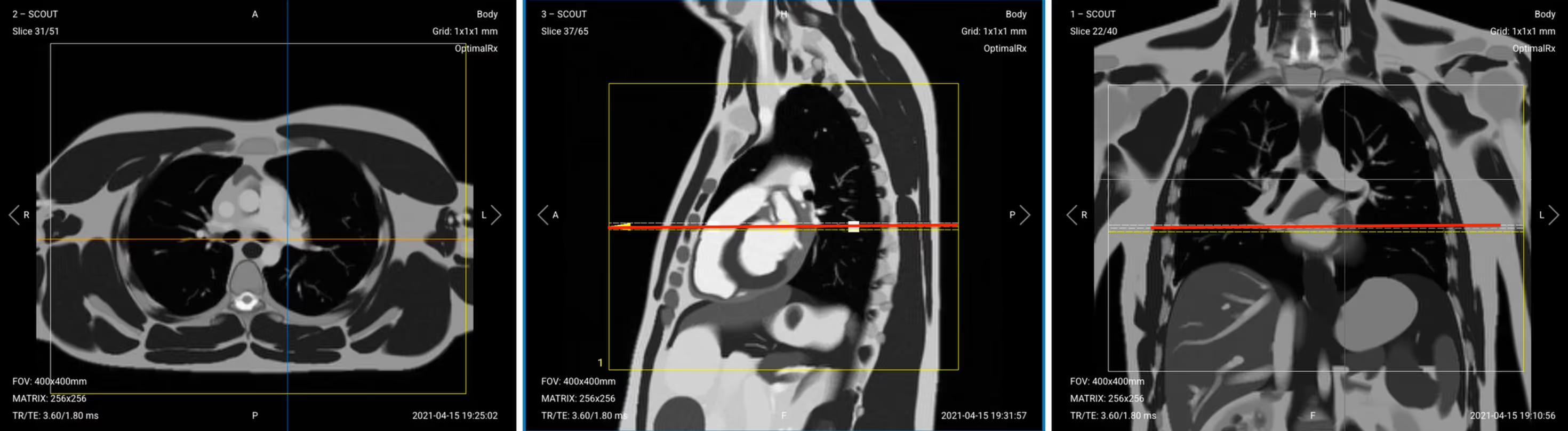
Planning Instructions:
Parameters for Bright Blood (Intra-Cardiac Anatomy, IR-TSE):
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 1.2–1.8 ms | Very short TE reduces susceptibility and banding artifacts in bSSFP and preserves blood nulling accuracy. |
| Repetition Time (TR) | 4.0–6.0 ms | Very short TR maintains the steady-state signal in bSSFP and supports rapid image acquisition. |
| Inversion Time (TI) | 800–900 ms | TI is timed to null the blood signal based on its T1 value at 1.5 T. |
| Field-of-View (FOV) | 380 × 320 mm | Covers the entire heart and mediastinum with acceptable resolution and minimizing aliasing. |
| Matrix | 192 × 256 | Medium matrix size balances spatial resolution, high SNR, and scan speed. Ideal for cardiac anatomy. |
| Foldover Direction (Phase) | Anterior-to-Posterior (AP) | Reduces motion artifacts from cardiac or respiratory motion, which typically occur in the superior-inferior direction. |
| Number of Slices | 25–40 | Ensures coverage from lung apices through the diaphragm to capture the full heart and mediastinum. |
| Slice Thickness | 6–8 mm | Thick enough for full myocardial coverage with good SNR; thinner slices may lose signal in bSSFP. |
| Slice Gap | 1–2 mm | Thin gaps reduce crosstalk and ensure full anatomical coverage without losing detail between slices. |
| NEX / Averages | 1–2 | One average keeps scan time short; a second average may improve SNR if motion is an issue. |
| Turbo Factor / ETL | N/A | Not applicable for bSSFP, which uses single-shot or segmented GRE readout rather than TSE. |
| Bandwidth | 192,000 Hz | High bandwidth shortens TE and reduces susceptibility and flow artifacts common in cardiac imaging. |
| Flip Angle | 50–70° | Optimized to enhance contrast between myocardium and suppressed blood signal while preserving SNR. |
| Fold-over Suppression | Yes | Prevents aliasing from arms, chest wall, or posterior structures entering the FOV. |
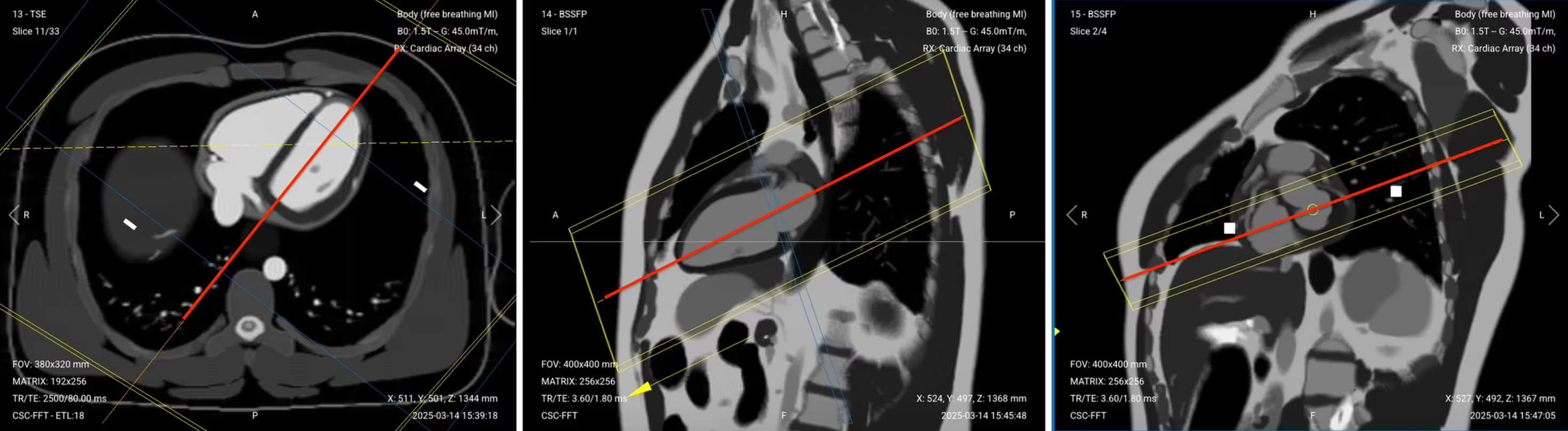
This localizer helps us plan the actual diagnostic sequences by capturing a preliminary view of the left atrium and left ventricle.
✅ Correct Planning:
Planning Instructions:
Parameters for Pseudo 2-Chamber View (bSSFP):
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 1.8 ms | Very short TE minimizes banding artifacts and enhances blood–myocardium contrast in bSSFP. |
| Repetition Time (TR) | 3.6 ms | Very short TR maintains steady-state magnetization for high SNR and bright-blood contrast. |
| Field-of-View (FOV) | 400 × 400 mm | Wide FOV ensures full coverage of the heart in oblique long-axis orientation. |
| Matrix | 256 × 256 | High matrix provides sharp in-plane resolution while maintaining fast scan times. |
| Foldover Direction (Phase) | Anterior-to-Posterior (AP) | Reduces wrap artifacts from lateral chest structures and aligns phase with respiratory motion. |
| Slice Thickness | 6–8 mm | Thick slices provide good coverage and SNR for planning or quick anatomical overview. |
| Slice Gap | 1–2 mm | Small gap prevents overlap and ensures complete coverage for stack planning. |
| Number of Slices | 3–4 | Enough slices to cover the pseudo 2-chamber view or enable quick scout imaging. |
| NEX / Averages | 1–2 | One average is standard; a second can help if motion or noise is present. |
| Bandwidth | 100,000 Hz | High bandwidth shortens TE and limits susceptibility and off-resonance artifacts. |
| Flip Angle | 50–70° | Balanced to maximize contrast between blood and myocardium in bSSFP imaging. |
| Fold-over Suppression | Yes | Prevents wrap-around artifacts from arms or posterior chest wall into the image. |
✅ Pseudo 2-Chamber View – Correct Image Example:

Things to Look for:
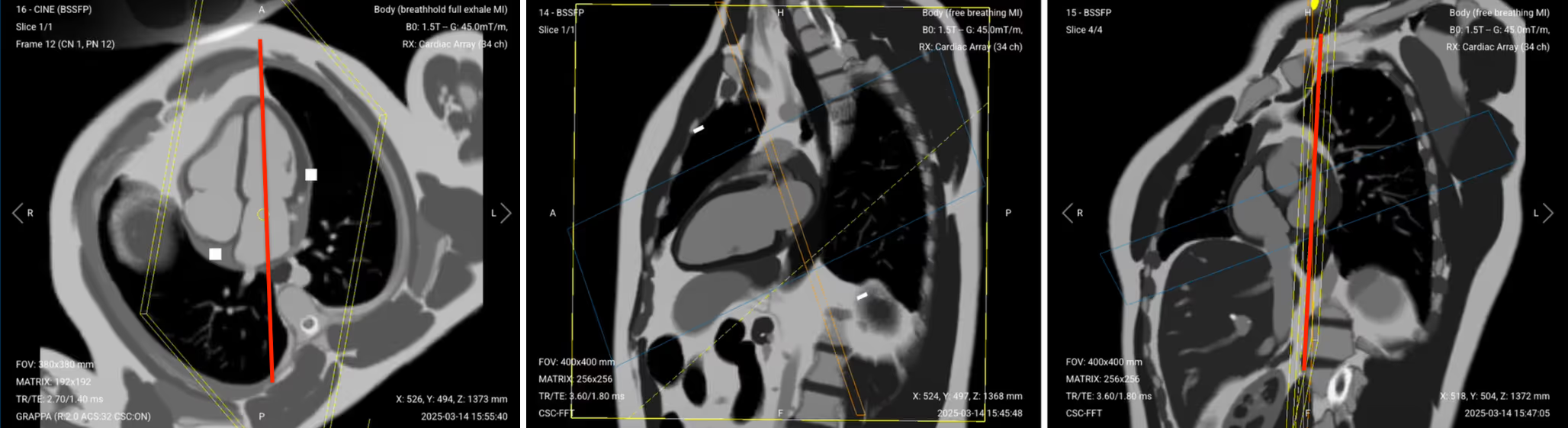
This localizer creates a perpendicular reference to the two-chamber view for planning the cine sequences. This stack helps identify structures to exclude later when refining the final 2-chamber view.
✅ Correct Planning:
Planning Instructions:
Parameters for Pseudo Short-Axis (SAX) View (bSSFP):
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 1.8 ms | Short TE minimizes banding artifacts and enhances blood–myocardium contrast in bSSFP. |
| Repetition Time (TR) | 3.6 ms | Short TR maintains steady-state magnetization for high SNR and bright-blood contrast. |
| Field-of-View (FOV) | 400 × 400 mm | Wide FOV ensures full heart coverage in oblique short-axis orientation. |
| Matrix | 256 × 256 | High matrix provides sharp in-plane resolution while maintaining fast scan times. |
| Foldover Direction (Phase) | Right-to-Left (RL) | Aligns phase with the short-axis view to avoid wrap-around artifacts from anterior/posterior chest. |
| Number of Slices | 3–4 | Captures enough slices to view the heart along the mitral valve plane and surrounding levels. |
| Slice Thickness | 6–8 mm | Thick slices provide good coverage and SNR for quick structural planning. |
| Slice Gap | 1–2 mm | Small gap avoids overlap while ensuring full coverage through the short-axis level. |
| NEX / Averages | 1–2 | One average is typical; two improves robustness in motion-prone areas. |
| Bandwidth | 100,000 Hz | High bandwidth shortens TE and reduces off-resonance and susceptibility artifacts. |
| Flip Angle | 50–70° | Balanced to optimize contrast between bright blood and myocardium in bSSFP. |
| Fold-over Suppression | Yes | Prevents wrap-around artifacts from adjacent anatomy like arms or lateral chest wall. |
✅ Pseudo SAX View – Correct Image Example:
.avif)
Things to Look for:
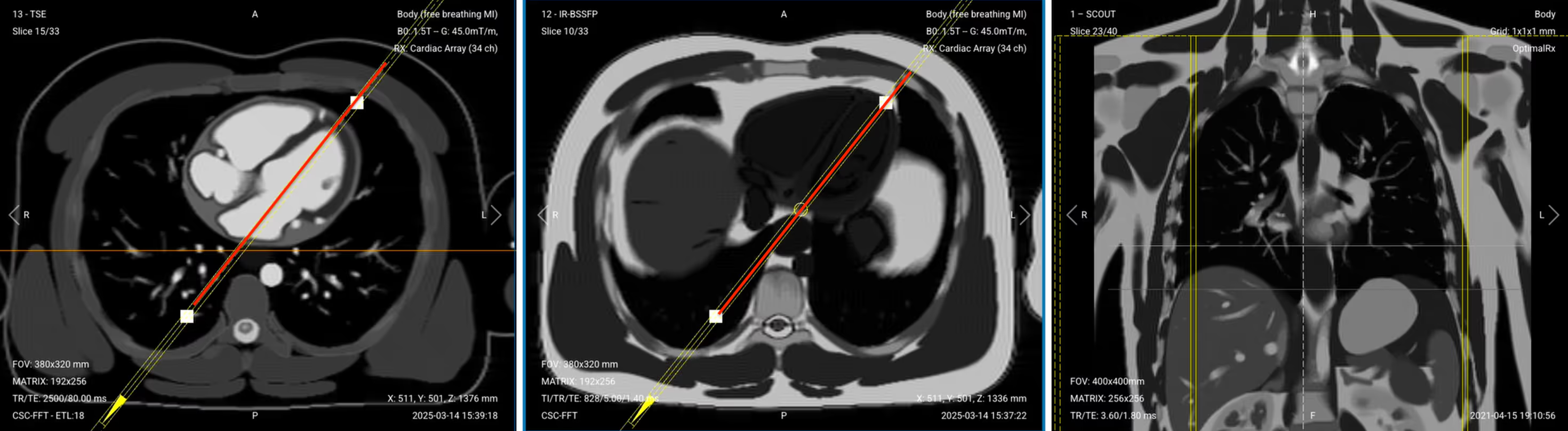
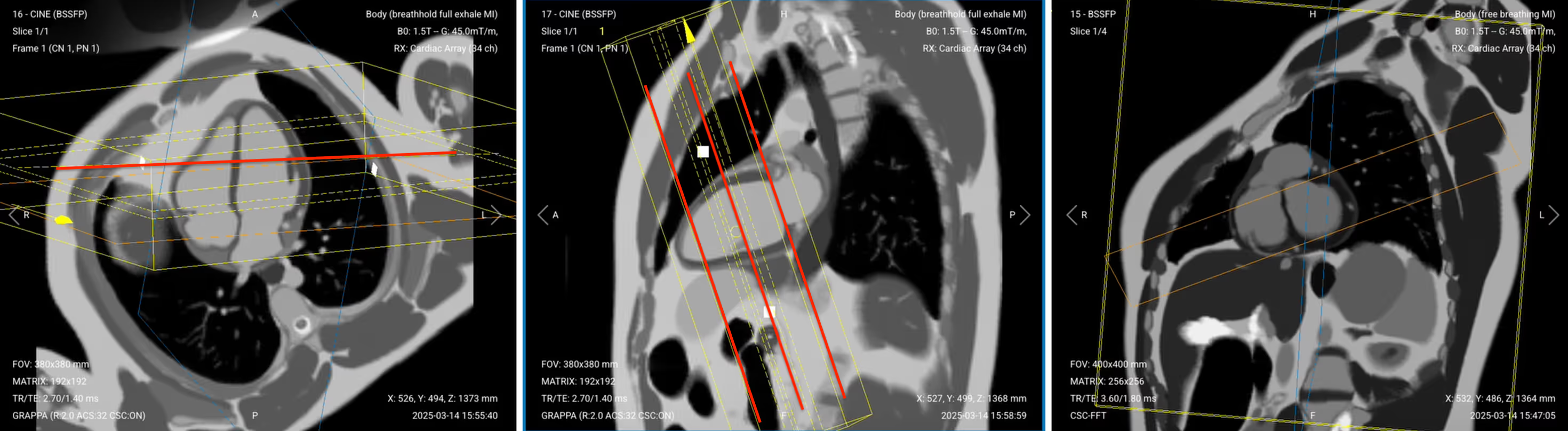
This diagnostic view shows all four heart chambers simultaneously, allowing assessment of their relationship.
✅ Correct Planning:
Planning Instructions:
Copy the slice position from the 2-chamber pseudo view as a starting point, then refine it to acquire the full 4-chamber view.
Use the mitral valve, left ventricle apex, and right ventricle apex as key anatomical references.
Align the slices as follows:
Axial localizer: Keep same as in pseudo 2-chamber. Ensure the slice passes through the mitral valve and continues to the apex of the left ventricle, forming a clean long-axis line through both left-sided chambers.
Sagittal 2-chamber pseudo: Adjust the slice to pass through the center of the mitral valve and extend down to the apex of the left ventricle.
Coronal SAX pseudo:
Tilt the slice so it runs below the aortic root and cuts through the right ventricle apex. Angle should intersect the full width of both atria and ventricles.
Scroll through coronal short-axis images to locate the slice where the left ventricular myocardium forms a complete ring (“black donut”). Make sure the 4-chamber cut passes through the center of this donut.

Confirm you see the classic “snowman” appearance: pulmonary artery (head), aorta (body), and left atrium (legs).

Set the fold-over direction (phase encoding) to anterior–posterior to reduce motion and metal artifacts, especially near implanted devices.
For patients with pacemakers or loop recorders, elevate the left arm above the head to reduce artifact interference during cine imaging.
Parameters for 4-Chamber Cine Imaging (SSFP):
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 1.4 ms | Very short TE minimizes banding and flow artifacts while preserving sharp contrast between blood and myocardium. |
| Repetition Time (TR) | 2.7 ms | Very short TR maintains steady-state for bSSFP and ensures smooth cine playback with high frame rate. |
| Field-of-View (FOV) | 380 × 380 mm | Sufficient coverage to capture the entire heart, including atria and ventricles. |
| Matrix | 192 × 192 | Medium matrix balances spatial resolution and temporal resolution for dynamic imaging. |
| Foldover Direction (Phase) | Anterior-to-Posterior (AP) | Aligns with chest motion and reduces wrap-around artifacts from lateral structures. |
| Number of Slices | 1 | Single slice used for dynamic 4-chamber cine to assess wall motion and valve function. |
| Slice Thickness | 6–8 mm | Thick enough for good SNR and full myocardial wall coverage in motion imaging. |
| Slice Gap | 1–2 mm | Allows spacing between multiple cine planes if needed for stack or reformatting. |
| NEX / Averages | 1–2 | One average provides adequate SNR for cine; a second helps if motion artifacts are present. |
| Bandwidth | 120,000 Hz | High bandwidth reduces chemical shift and flow artifacts, allowing for rapid echo spacing and clean image quality. |
| Flip Angle | 50–70° | Optimized to maximize contrast between bright blood and myocardium while maintaining signal stability in SSFP. |
| Fold-over Suppression | Yes | Prevents aliasing from anterior chest wall or posterior structures entering the image. |
| Parallel Imaging | GRAPPA | Reduces scan time and echo train length, improving temporal resolution while maintaining image quality. |
| Acceleration Factor | 2–3 | Speeds up acquisition by under-sampling in phase direction; factor of 2–3 balances speed and artifact risk. |
The 2-Chamber view focuses specifically on the left atrium and left ventricle.
✅ Correct Planning:
Planning Instructions:
Parameters for 2-Chamber Cine Imaging (SSFP):
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 1.4 ms | Very short TE minimizes banding and flow artifacts while preserving sharp contrast between blood and myocardium. |
| Repetition Time (TR) | 2.7 ms | Very short TR maintains steady-state for bSSFP and ensures smooth cine playback with high frame rate. |
| Field-of-View (FOV) | 380 × 380 mm | Sufficient coverage to capture the entire heart, including atria and ventricles. |
| Matrix | 192 × 192 | Medium matrix balances spatial resolution and temporal resolution for dynamic imaging. |
| Foldover Direction (Phase) | Anterior-to-Posterior (AP) | Aligns with chest motion and reduces wrap-around artifacts from lateral structures. |
| Number of Slices | 1 | Single slice used for dynamic 2-chamber cine to assess wall motion and valve function. |
| Slice Thickness | 6–8 mm | Thick enough for good SNR and full myocardial wall coverage in motion imaging. |
| Slice Gap | 1–2 mm | Allows spacing between multiple cine planes if needed for stack or reformatting. |
| NEX / Averages | 1–2 | One average provides adequate SNR for cine; a second helps if motion artifacts are present. |
| Bandwidth | 120,000 Hz | High bandwidth reduces chemical shift and flow artifacts, allowing for rapid echo spacing and clean image quality. |
| Flip Angle | 50–70° | Optimized to maximize contrast between bright blood and myocardium while maintaining signal stability in SSFP. |
| Fold-over Suppression | Yes | Prevents aliasing from anterior chest wall or posterior structures entering the image. |
| Parallel Imaging | GRAPPA | Reduces scan time and echo train length, improving temporal resolution while maintaining image quality. |
| Acceleration Factor | 2–3 | Speeds up acquisition by under-sampling in phase direction; factor of 2–3 balances speed and artifact risk. |
The 3-Chamber view shows the left ventricular outflow tract (LVOT), providing important information about the aorta.
✅ Correct Planning:

Planning Instructions:
Parameters for LVOT / 3-chamber Cine Imaging (SSFP):
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 1.4 ms | Very short TE minimizes banding and flow artifacts while preserving sharp contrast between blood and myocardium. |
| Repetition Time (TR) | 2.7 ms | Very short TR maintains steady-state for bSSFP and ensures smooth cine playback with high frame rate. |
| Field-of-View (FOV) | 380 × 380 mm | Sufficient coverage to capture the entire heart, including atria and ventricles. |
| Matrix | 192 × 192 | Medium matrix balances spatial resolution and temporal resolution for dynamic imaging. |
| Foldover Direction (Phase) | Anterior-to-Posterior (AP) | Aligns with chest motion and reduces wrap-around artifacts from lateral structures. |
| Number of Slices | 1 | Single slice used for dynamic 3-chamber cine to assess wall motion and valve function. |
| Slice Thickness | 6–8 mm | Thick enough for good SNR and full myocardial wall coverage in motion imaging. |
| Slice Gap | 1–2 mm | Allows spacing between multiple cine planes if needed for stack or reformatting. |
| NEX / Averages | 1–2 | One average provides adequate SNR for cine; a second helps if motion artifacts are present. |
| Bandwidth | 120,000 Hz | High bandwidth reduces chemical shift and flow artifacts, allowing for rapid echo spacing and clean image quality. |
| Flip Angle | 50–70° | Optimized to maximize contrast between bright blood and myocardium while maintaining signal stability in SSFP. |
| Fold-over Suppression | Yes | Prevents aliasing from anterior chest wall or posterior structures entering the image. |
| Parallel Imaging | GRAPPA | Reduces scan time and echo train length, improving temporal resolution while maintaining image quality. |
| Acceleration Factor | 2–3 | Speeds up acquisition by under-sampling in phase direction; factor of 2–3 balances speed and artifact risk. |
The Short-Axis stack provides multiple slices from the base to the apex of the heart, allowing for volumetric measurements.
✅ Correct Planning:
Planning Instructions:
Parameters for Short-Axis (SAX) Stack Cine (SSFP):
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 1.4 ms | Very short TE minimizes banding and flow artifacts while preserving sharp contrast between blood and myocardium. |
| Repetition Time (TR) | 2.7 ms | Very short TR maintains steady-state for bSSFP and ensures smooth cine playback with high frame rate. |
| Field-of-View (FOV) | 380 × 380 mm | Sufficient coverage to capture the entire heart, including atria and ventricles. |
| Matrix | 192 × 192 | Medium matrix balances spatial resolution and temporal resolution for dynamic imaging. |
| Foldover Direction (Phase) | Foot-to-Head (FH) / Superior-to-Inferior | FH avoids wrap from chest/arms into the heart region. Aligns with natural body length to minimize respiratory artifacts. |
| Number of Slices | 9–12 | Depending on patient’s heart size. Use 10 slices for average adult cases. |
| Slice Thickness | 7–8 mm | Thick enough for full heart coverage without large gaps. This improves SNR while keeping resolution acceptable. |
| Slice Gap | 2–3 mm | Set so that Gap + Thickness = 10. For example, if slice thickness is 7 mm, set slice gap to 10 – 7 = 3. |
| NEX / Averages | 1–2 | One average provides adequate SNR for cine; a second helps if motion artifacts are present. |
| Bandwidth | 120,000 | High bandwidth reduces chemical shift and flow artifacts, allowing for rapid echo spacing and clean image quality. |
| Flip Angle | 50–70° | Optimized to maximize contrast between bright blood and myocardium while maintaining signal stability in SSFP. |
| Fold-over Suppression | Yes | Prevents aliasing from anterior chest wall or posterior structures entering the image. |
| Parallel Imaging | GRAPPA | Reduces scan time and echo train length, improving temporal resolution while maintaining image quality. |
| Acceleration Factor | 2–3 | Speeds up acquisition by under-sampling in phase direction; factor of 2–3 balances speed and artifact risk. |
The table below lists the 6 common cardiac artifacts, and what techniques you can use to avoid them:
| Artifacts | Solution – How to Avoid It |
|---|---|
| Motion | Use ECG-gating to synchronize image acquisition with the patient’s cardiac cycle and reduce heart motion. |
| Breathing | Instruct patients to hold their breath during imaging. Use breath-hold sequences when possible. |
| ECG mis-triggering | Use real-time cine imaging to minimize the impact of poor ECG signals or arrhythmias. |
| Flow | Align the phase encoding direction 90° to major vessels to reduce ghosting from blood flow. |
| Susceptibility | Increase the bandwidth to shorten readout time and reduce distortion from magnetic field variations. |
| Wrap-around | Use fold-over suppression or phase oversampling to prevent anatomy outside the FOV from overlapping. |
Finally, we will review the images to ensure all the anatomical information we need is clear.
In a cardiac viability MRI focused on morphology and function, these structures must be clearly visible:
Below, we will go through all the different image contrasts and explain their specific role in imaging the heart.
The black blood uses an inversion recovery to null the signal from flowing blood. This makes moving blood appear black while static tissues like myocardium and fat appear gray/bright. The strong contrast lets us inspect extra-cardiac anatomy, vessel walls, and tissue boundaries.
In cardiac viability imaging, black blood is vital for assessing morphology. It helps identify pericardial thickening, pleural effusion, and fat infiltration. It also confirms proper planning and helps visualize lung bases, diaphragm, and adjacent chest anatomy.
✅ Black Blood IR-TSE – Correct Image Example:

Things to Look for in Black Blood:
This sequence uses an inversion pulse with a TSE readout, which makes flowing blood appear bright while suppressing background tissue. It shows the blood pool, chamber size, and great vessels clearly, with sharp contrast and reduced motion artifacts.
In viability protocols, bright blood is also used to examine morphology, specifically intra-cardiac anatomy, dilation, septal shift, and large effusions.
✅ Bright Blood IR-TSE – Correct Image Example:

Things to Look for in Bright Blood:
Cine imaging uses a fast, ECG-gated sequence to capture the heart through multiple cardiac phases. It shows the heart beating like a movie across systole and diastole.
Cine is the gold standard for evaluating global function, such as ejection fraction, wall motion, and ventricular contractility.
In cardiac viability studies, cine images are a must to:
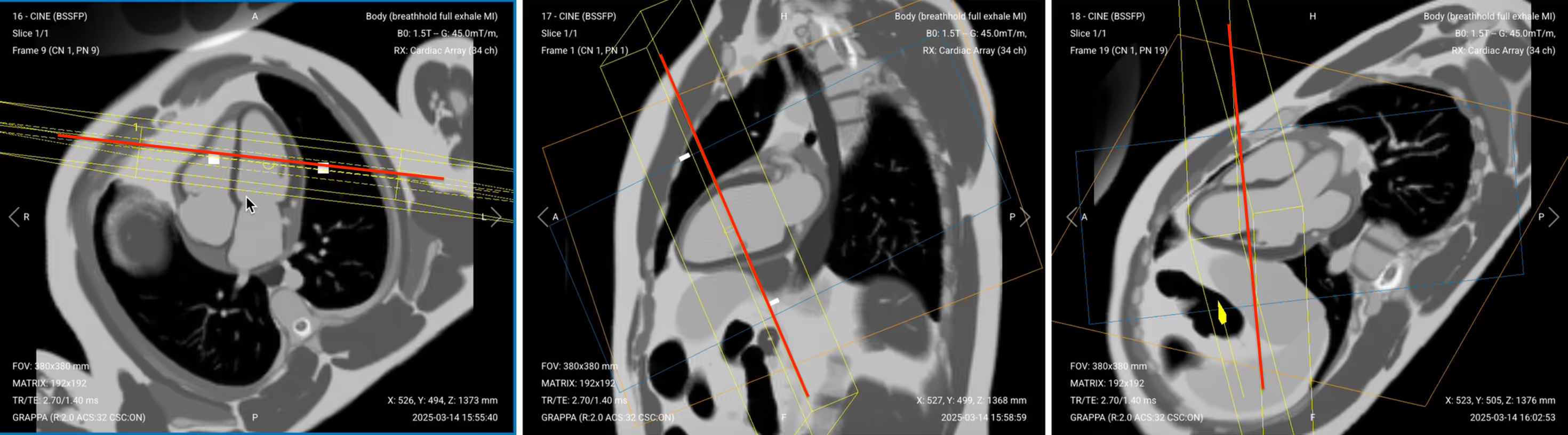
✅ 4-Chamber Cine SSFP of the Heart – Correct Image Example:

Note that the 4-chamber cine image above shows a minor wrapping artifact at its top. But since it doesn’t interfere with the anatomy of the heart, it still meets diagnostic quality.
Things to Look for in 4-Chamber Cine:
✅ 2-Chamber Cine SSFP of the Heart – Correct Image Example:

Things to Look for in 2-Chamber Cine:
✅ 3-Chamber (LVOT) Cine SSFP of the Heart – Correct Image Example:

Things to Look for in 3-Chamber (LVOT) Cine:
✅ Short-Axis Stack Cine of the Heart – Correct Image Example:

Things to Look for in Short-Axis Stack Cine:
Before finishing a cardiac viability MRI, always check these 6 points to ensure diagnostic quality:
These checks help confirm scan success before contrast or treatment decisions.
This completes the planning phase of our cardiac viability MRI protocol focusing on function and morphology.
In Part 2, we'll cover cardiac tissue characterization with perfusion and late gadolinium enhancement sequences to complete the full viability study.