
Get FREE Weekly MRI Content

This step-by-step guide is for MRI students, radiographers, and technologists who wish to improve their planning skills and master the thoracic spine MRI protocol.
What you will learn:
The thoracic spine is heavily affected by breathing and cardiac motion, making motion artifacts the biggest problem. We're also imaging near air-filled lungs with low proton density, creating challenging conditions for signal quality. This makes SNR our second priority. Resolution comes third, though we still need good detail to see ligaments, disc herniations, and spinal cord structures.
These sequences provide fast acquisition with excellent soft tissue contrast. They work well for T2, T1, and STIR weightings, helping us assess the thoracic spine and detect common pathologies while keeping scan time short.
| Artifacts | Solution – How to Avoid It |
|---|---|
| Motion artifacts | Use saturation bands placed anterior to the spine to suppress cardiac and respiratory motion. |
| Susceptibility artifacts | Use spin echo sequences instead of gradient echo to reduce sensitivity to magnetic field inhomogeneities near air-tissue interfaces. |
| Flow artifacts | Align the phase encoding direction foot-to-head with CSF flow to reduce flow-related signal loss. |
| Chemical shift artifacts | Increase the bandwidth to reduce spatial displacement between fat and water signals. |
| Wrap-around artifacts | Activate fold-over suppression to prevent anatomy outside the field of view from overlapping. |
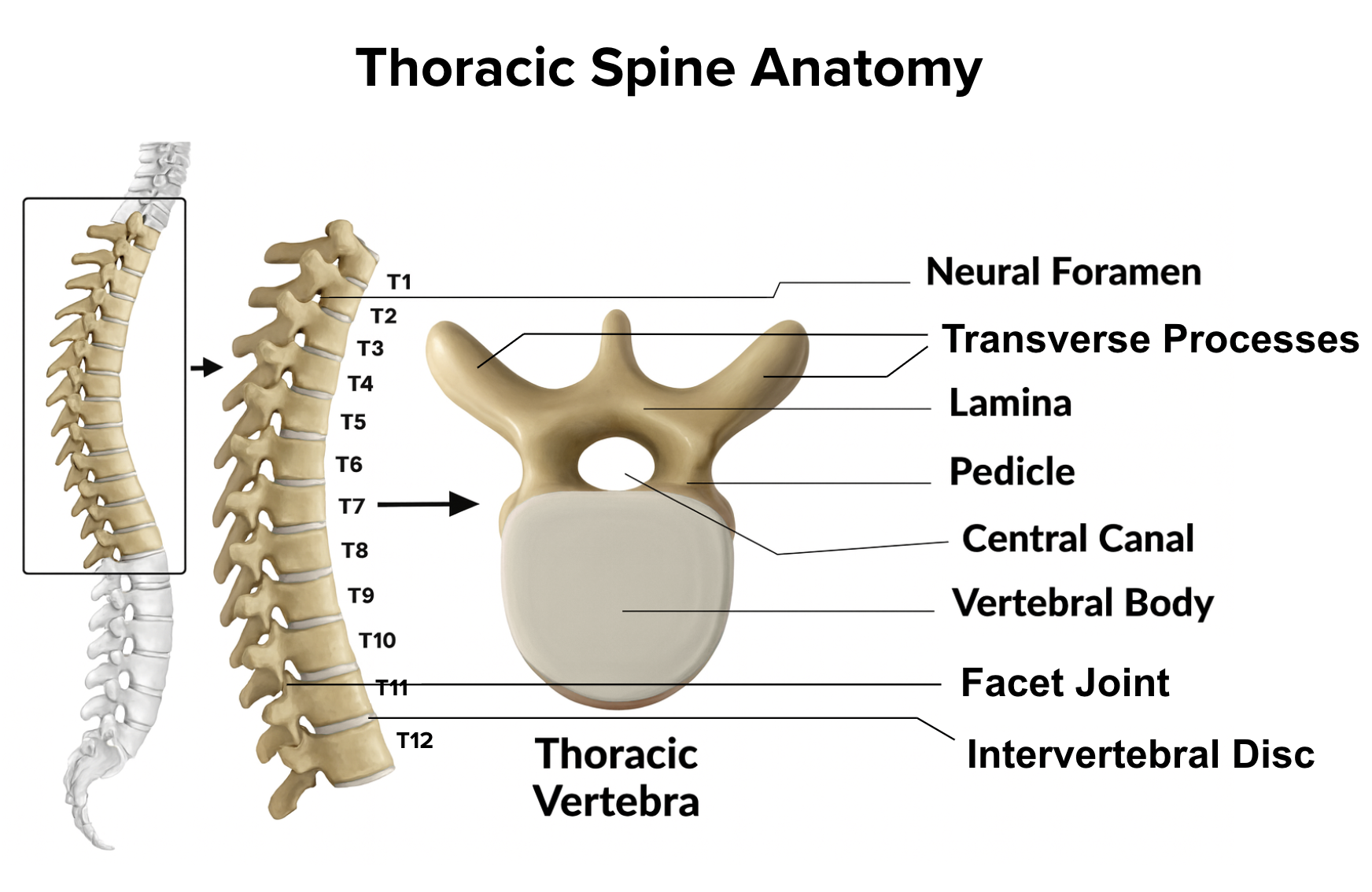
The thoracic spine is the mid-back region that bridges the cervical and lumbar spine. It consists of 12 thoracic vertebrae (T1–T12) and serves as the structural foundation for the rib cage. This region protects vital organs, supports the upper body, and houses the spinal cord and nerve roots.
Because of its proximity to the heart and lungs, the thoracic spine is particularly susceptible to motion artifacts from breathing and cardiac pulsation. It's also a common source of pain, neurological symptoms, and pathologies affecting the spinal cord and surrounding structures.
In MRI, we always face a trade-off between 3 key metrics:
Improving one of these metrics reduces the performance of the others. To decide what trade-offs to make, we must consider the needs of each clinical situation.
For thoracic spine MRIs, we face these challenges:
Therefore, we typically:
Short scan times reduce the risk of motion blur from breathing and cardiac pulsation. Strong SNR helps us distinguish between the spinal cord, cerebrospinal fluid, and surrounding tissues clearly. We need good resolution to see fine structures, but we can't push it so high that it destroys our scan time or SNR.

The thoracic spine MRI study can help us diagnose a wide range of health conditions. The table below lists some of the most common conditions, and what pulse sequences that reveal them:
| Common Thoracic Spine Conditions | Clearly Seen on Sequence | Why This Sequence? |
|---|---|---|
|
Degenerative and Soft Tissue Disorders: • Disc herniation • Disc bulges • Degenerative disc disease |
T2 TSE | Highlights water-rich tissues like CSF, and soft-tissue, and inflamed discs (which appear bright due to high water content). Herniated discs appear as bulges or extrusions that may compress the spinal cord or nerve roots. |
|
Structural and Neoplastic Changes: • Spinal fractures • Spinal tumors • Stenosis • Spinal cord compression |
T1 TSE | Provides clear anatomical detail of vertebral bodies and spinal cord. Shows cord compression clearly and detects bone marrow changes from fractures or tumors.Provides clear anatomical detail of vertebral bodies and spinal cord. Shows cord compression clearly and detects bone marrow changes from fractures or tumors. |
|
Inflammatory and Infectious Conditions: • MS plaques • Infections: • Abscesses • Inflammatory conditions |
STIR TSE | Suppresses fat signals completely, making water-rich tissues stand out even clearer than on T2. This makes STIR ideal for detecting subtle edema, inflammation, and infections, where increased water content would otherwise be obscured by fat. Provides high lesion visibility for inflammatory conditions. |
The step-by-step guide below will show you how to set up and perform a thoracic spine MRI protocol in practice.
We will perform the protocol in 3 parts:
Lay the patient feet-first and supine (on their back) with the thoracic region aligned at the scanner's isocenter.
Using a feet-first position makes the scan feel less claustrophobic for the patient, which reduces the risk of motion artifacts.
Place a dedicated thoracic spine coil at the patient's back. This coil ensures you get full coverage of the thoracic region and delivers strong signal acquisition for clear images. The coil should be positioned to cover all 12 thoracic vertebrae.
✅ Correct Patient Positioning:

Once the patient is in place, review your scanner's hardware settings.
In this guide, we will use the following settings:
| Scanner Setting | Value | Why This Value |
|---|---|---|
| Magnetic field strength | 1.5 or 3 T | 1.5 T enables high Signal-to-Noise Ratio, which gives superior image quality. 3T provides roughly double the signal for improved resolution or reduced scan time. |
| Maximum gradient strength | 45 mT/m | Enables faster acquisitions while preserving high image quality. |
This hardware setup is widely used in clinical practice. It balances acquisition time, image quality, and patient comfort.
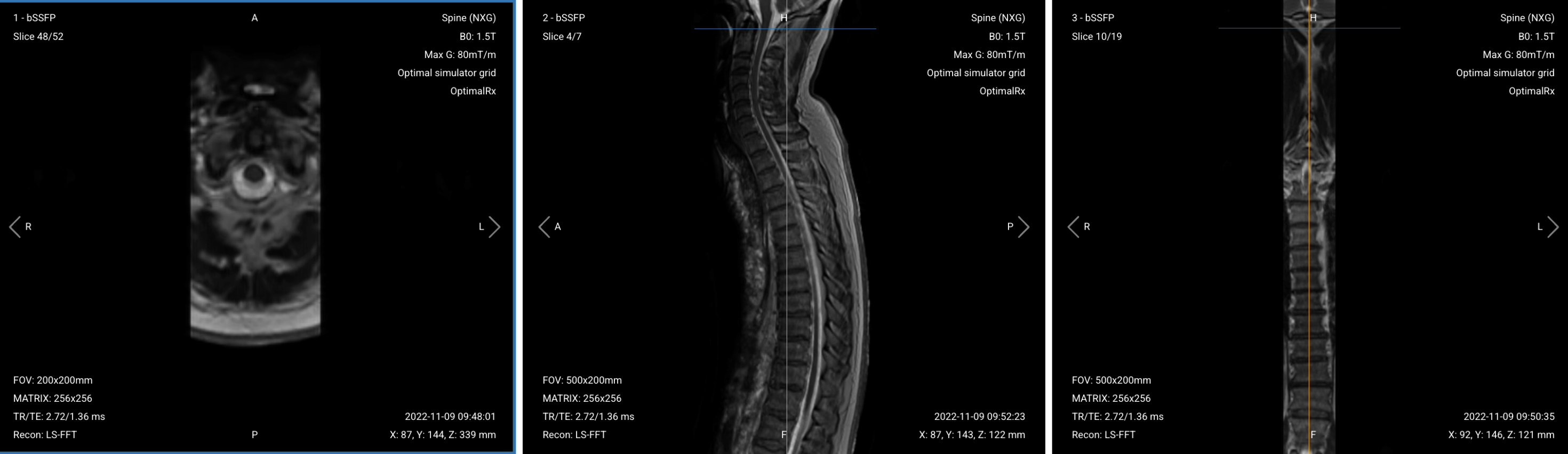
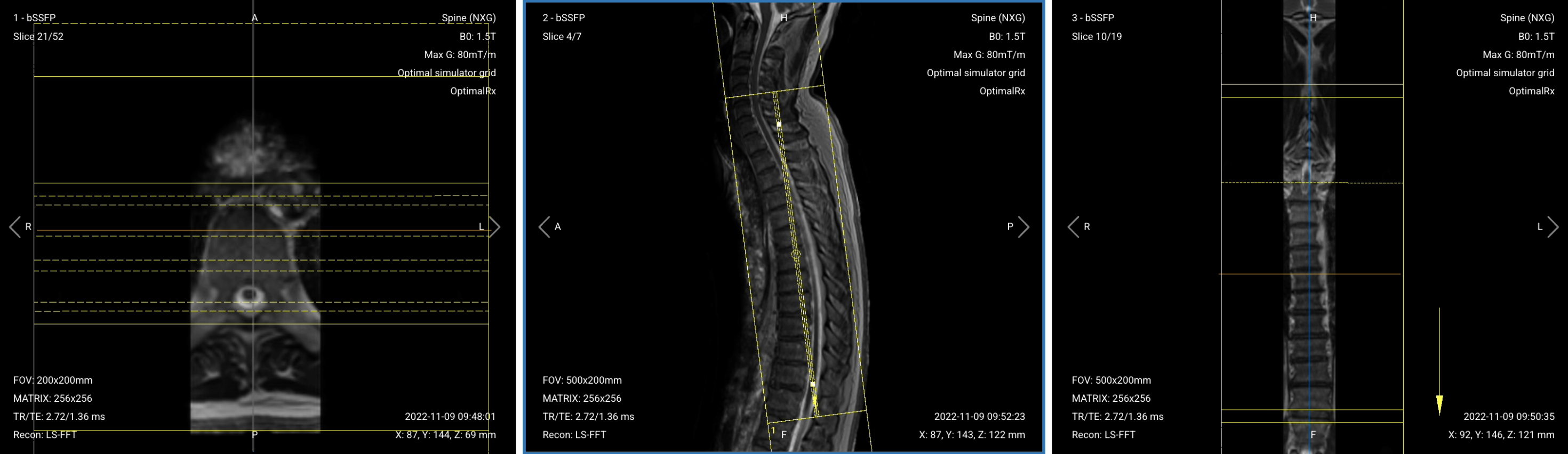
Before we can perform any MRI protocol, we must always capture initial localizer images of the patient. These images act as a guide for planning the detailed scans we will perform next.
We should always capture localizers in three planes:
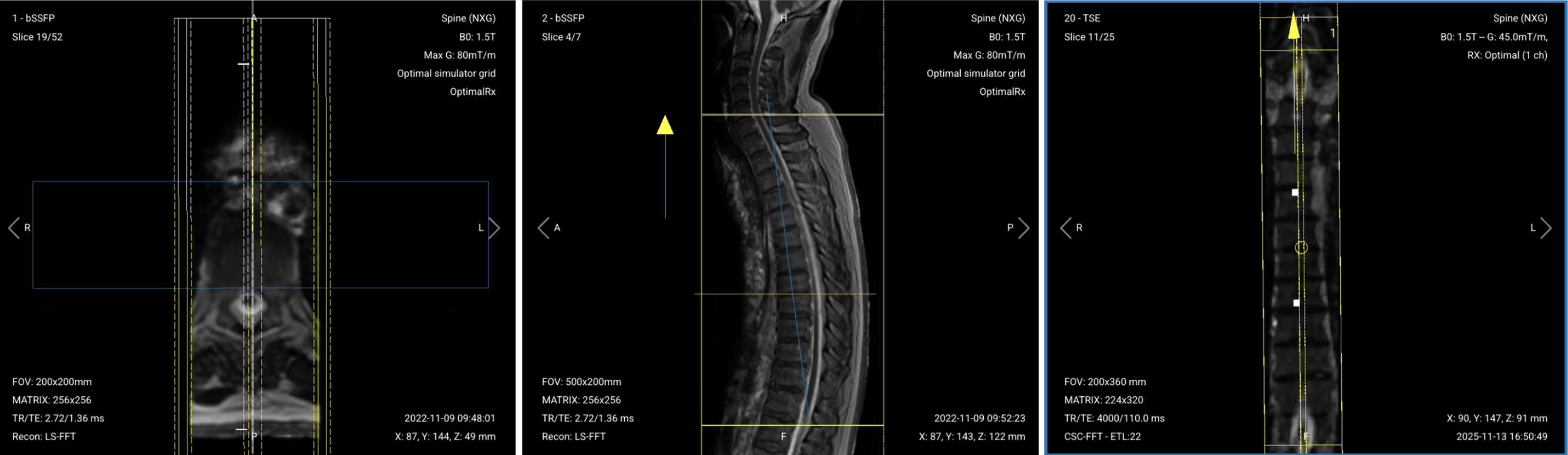
Once acquired, upload the initial localizer images into the three viewports.
Then, scroll through each of the image stacks to locate a central slice that clearly shows the anatomy of the thoracic spine.
✅ Correct Setup of Localizer Images for Thoracic Spine MRI:
When all preparations are ready, we can start planning and acquiring the protocol sequences.
Let's go through the pulse sequences a standard thoracic spine MRI protocol includes, why we perform them, and how to set them up.
We mainly use Turbo/Fast Spin Echo sequences for this study. These sequences provide fast acquisition with excellent soft tissue contrast. They work well for creating multiple contrasts, including T2, T1, and inversion recovery for fat suppression. This helps us assess the thoracic spine and detect common pathologies while keeping scan time short.
In the sections below, we go through how to plan and set up each sequence.
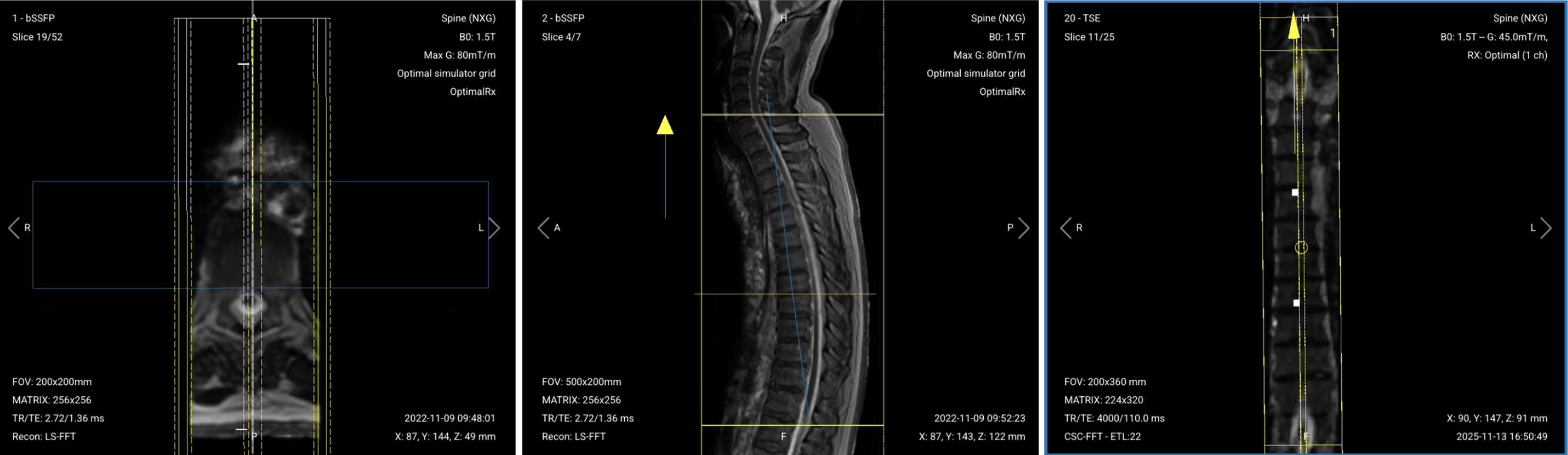
✅ Correct Planning:
Planning Instructions:
Parameters for Coronal T2 TSE:
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 100–120 ms | Longer TE is required for T2 contrast. |
| Repetition Time (TR) | 4,000–6,000 ms | Longer TR is required for T2 contrast. |
| Field-of-View (FOV) | 200 × 360 mm | Rectangular FOV optimized for the thoracic spine's vertical extent, covering superior-to-inferior while minimizing anterior-posterior to reduce scan time. |
| Matrix | 224 × 320 | Medium matrix size to get sufficient resolution and detail while maintaining short scan time and high SNR. |
| Foldover Direction (Phase) | Foot-to-Head (FH) / Superior-to-Inferior | To align with cerebrospinal fluid flow and reduce flow artifacts. |
| Number of Slices | 22–26 | Enough slices to fully cover all 12 thoracic vertebrae. |
| Slice Thickness | 4 mm | Medium thickness to get good resolution without sacrificing scan time or SNR. |
| Slice Gap | 0.4 mm | 10% of slice thickness to prevent crosstalk while ensuring continuity. |
| NEX / Averages | 1–2 | To get enough SNR while keeping scan time short. |
| Turbo Factor / ETL | 16–24 | Higher turbo factor to enhance T2 contrast and reduce scan time. |
| Bandwidth | 50,000 Hz | Medium bandwidth balances SNR with chemical shift artifact reduction. Lower than typical values to improve SNR in the challenging thoracic region. |
| Fold-over Suppression | Yes | To avoid aliasing or wrap-around artifacts. |
✅ Correct Planning:
Planning Instructions:
Parameters for Sagittal T2 TSE:
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 100–120 ms | Longer TE is required for T2 contrast. |
| Repetition Time (TR) | 4,000–6,000 ms | Longer TR is required for T2 contrast. |
| Field-of-View (FOV) | 200 × 340 mm | Rectangular FOV optimized for the thoracic spine's vertical extent, covering superior-to-inferior while minimizing anterior-posterior to reduce scan time. |
| Matrix | 224 × 320 | Medium matrix size provides sufficient resolution while maintaining short scan time and high SNR. |
| Foldover Direction (Phase) | Foot-to-Head (FH) / Superior-to-Inferior | Aligns with cerebrospinal fluid flow to reduce flow artifacts. |
| Number of Slices | 14–18 | Enough slices to cover the thoracic spine from right to left. |
| Slice Thickness | 4 mm | Medium thickness provides good resolution without sacrificing scan time or SNR. |
| Slice Gap | 0.4 mm | 10% of slice thickness prevents crosstalk while ensuring continuity. |
| NEX / Averages | 1–2 | Provides enough SNR while keeping scan time short. |
| Turbo Factor / ETL | 16–24 | Higher turbo factor enhances T2 contrast and reduces scan time. |
| Bandwidth | 50,000 Hz | Medium bandwidth balances SNR with chemical shift artifact reduction. Lower than typical values to improve SNR in the challenging thoracic region. |
| Fold-over Suppression | Yes | Prevents aliasing or wrap-around artifacts. |
✅ Correct Planning:
Planning Instructions:
Parameters for Sagittal STIR TSE:
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 20–40 ms | Medium TE balances T2 weighting with inversion recovery effects. |
| Repetition Time (TR) | 3,000–5,000 ms | Long TR allows adequate T2 weighting while accommodating the inversion pulse. |
| Inversion Time (TI) | 130–150 ms | TI matches the fat null point at 1.5T, enabling robust fat suppression. |
| Field-of-View (FOV) | 200 × 340 mm | Rectangular FOV optimized for the thoracic spine's vertical extent, covering superior-to-inferior while minimizing anterior-posterior to reduce scan time. |
| Matrix | 224 × 320 | Medium matrix size provides sufficient resolution while maintaining short scan time and high SNR. |
| Foldover Direction (Phase) | Foot-to-Head (FH) / Superior-to-Inferior | Aligns with CSF flow to reduce flow-related artifacts. |
| Number of Slices | 14–18 | Covers the thoracic spine from right to left adequately. |
| Slice Thickness | 4 mm | Medium thickness gives good spatial resolution without excessive scan time. |
| Slice Gap | 0.4 mm | 10% of slice thickness prevents crosstalk while preserving continuity. |
| NEX / Averages | 1–2 | Provides adequate SNR while keeping the scan time reasonable. |
| Turbo Factor / ETL | 10–14 | Optimizes contrast and spatial resolution based on STIR’s echo time needs. |
| Bandwidth | 50,000 Hz | Medium bandwidth balances SNR with chemical shift artifact reduction. Lower than typical values to improve SNR in the challenging thoracic region. |
| Fold-over Suppression | Yes | Prevents wrap-around artifacts from surrounding thoracic structures. |
✅ Correct Planning:
.png)
Planning Instructions:
Parameters for Sagittal T1 TSE:
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 10–20 ms | Shorter TE is required for T1 contrast. |
| Repetition Time (TR) | 400–600 ms | Shorter TR is required for T1 contrast. |
| Field-of-View (FOV) | 200 × 340 mm | Rectangular FOV optimized for the thoracic spine's vertical extent, covering superior-to-inferior while minimizing anterior-posterior to reduce scan time. |
| Matrix | 224 × 320 | Medium matrix size provides sufficient resolution while maintaining short scan time and high SNR. |
| Foldover Direction (Phase) | Foot-to-Head (FH) / Superior-to-Inferior | Aligns with cerebrospinal fluid flow to reduce flow artifacts. |
| Number of Slices | 14–18 | Covers the thoracic spine from right to left adequately. |
| Slice Thickness | 4 mm | Medium thickness provides good resolution without increasing scan time too much. |
| Slice Gap | 0.4 mm | 10% of slice thickness prevents crosstalk while maintaining continuity. |
| NEX / Averages | 1–2 | Provides adequate SNR while keeping scan time reasonable. |
| Turbo Factor / ETL | 2–3 | Low turbo factor minimizes T2-weighting and preserves pure T1 contrast. |
| Bandwidth | 50,000 Hz | Medium bandwidth balances SNR with chemical shift artifact reduction. Lower than typical values to improve SNR in the challenging thoracic region. |
| Fold-over Suppression | Yes | Prevents wrap-around artifacts. |
| Saturation Bands | Yes | Placed anterior to the spine to suppress cardiac, respiratory, and vascular motion artifacts. |
✅ Correct Planning:
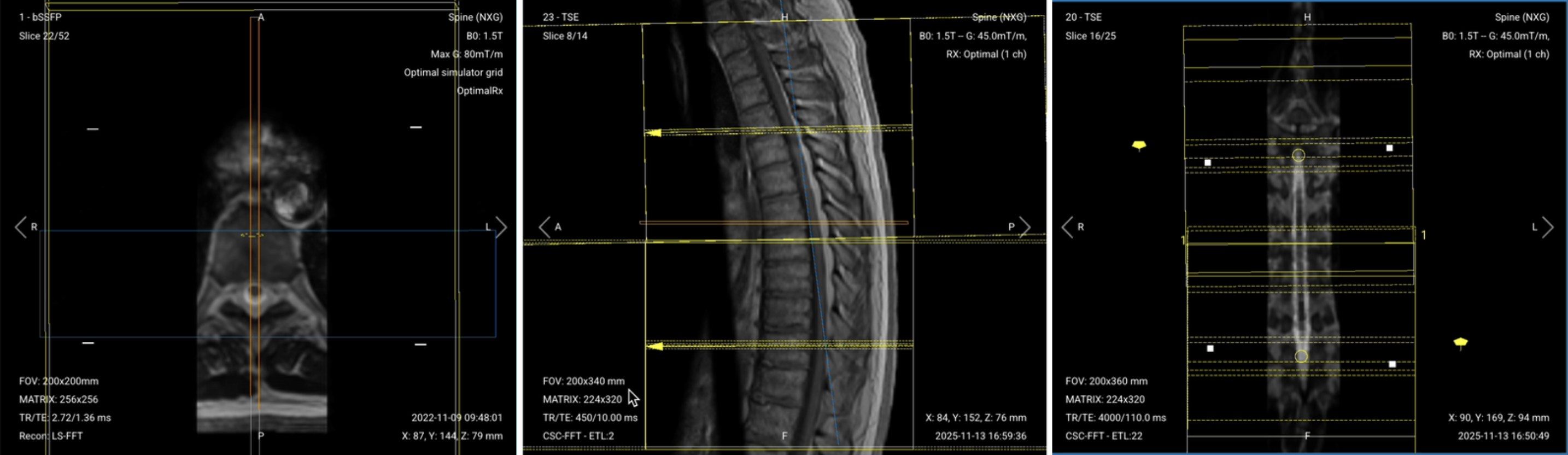
Planning Instructions:
Parameters for Axial T2 TSE:
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 100–120 ms | Longer TE is required for T2 contrast. |
| Repetition Time (TR) | 4,000–6,000 ms | Long TR is required for T2 contrast. |
| Field-of-View (FOV) | 180 × 200 mm | Small FOV focused on the thoracic spine region, minimizing unnecessary coverage to reduce scan time and optimize resolution. |
| Matrix | 224 × 224 | Medium matrix size provides good resolution with faster acquisition, balancing detail with scan time and SNR. |
| Foldover Direction (Phase) | Anterior-to-Posterior (AP) | Avoids motion artifacts from cardiac and respiratory movement. |
| Number of Slices | 50-70 (single stack) 30–40 per stack (double stack) |
Enough slices to cover all 12 thoracic vertebrae. |
| Slice Thickness | 4 mm | Medium thickness provides good anatomical detail without increasing scan time excessively. |
| Slice Gap | 0.4 mm | 10% of slice thickness prevents crosstalk while ensuring continuity. |
| NEX / Averages | 1–2 | Provides adequate SNR while controlling scan time. |
| Turbo Factor / ETL | 16–24 | Higher turbo factor enhances T2 contrast and reduces scan time. |
| Bandwidth | 50,000 Hz | Medium bandwidth balances SNR with chemical shift artifact reduction. Lower than typical values to improve SNR in the challenging thoracic region. |
| Fold-over Suppression | Yes | Prevents wrap-around artifacts. |
Parameters for Axial T1 TSE:
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 10–20 ms | Shorter TE is required for T1 contrast. |
| Repetition Time (TR) | 400–600 ms | Shorter TR is required for T1 contrast. |
| Field-of-View (FOV) | 180 × 200 mm | Small FOV focused on the thoracic spine region, minimizing unnecessary coverage to reduce scan time and optimize resolution. |
| Matrix | 224 × 224 | Medium matrix size provides good resolution with faster acquisition, balancing detail with scan time and SNR. |
| Foldover Direction (Phase) | Right-to-Left (RL) or Anterior-to-Posterior (AP) |
RL can be used if AP causes wrap artifacts. AP reduces cardiac and respiratory motion artifacts. |
| Number of Slices | 50-70 (single stack) 30–40 per stack (double stack) |
Enough slices to cover all 12 thoracic vertebrae. |
| Slice Thickness | 4 mm | Medium thickness balances anatomical detail with SNR and scan time. |
| Slice Gap | 0.4 mm | 10% of slice thickness prevents crosstalk while maintaining continuity. |
| NEX / Averages | 1–2 | Provides adequate SNR while keeping scan time efficient. |
| Turbo Factor / ETL | 2–3 | Low turbo factor minimizes T2-weighting and preserves pure T1 contrast. |
| Bandwidth | 50,000 Hz | Medium bandwidth balances SNR with chemical shift artifact reduction. Lower than typical values to improve SNR in the challenging thoracic region. |
| Fold-over Suppression | Yes (if using AP phase) Optional (if using RL phase) |
Needed with AP phase to prevent wrap-around artifacts. May be optional with RL depending on patient width and positioning. |
The table below lists the 5 common thoracic spine artifacts, and what techniques you can use to avoid them:
| Artifacts | Solution – How to Avoid It |
|---|---|
| Motion artifacts | Use saturation bands placed anterior to the spine to suppress cardiac and respiratory motion. |
| Susceptibility artifacts | Use spin echo sequences instead of gradient echo to reduce sensitivity to magnetic field inhomogeneities near air-tissue interfaces. |
| Flow artifacts | Align the phase encoding direction foot-to-head with CSF flow to reduce flow-related signal loss. |
| Chemical shift artifacts | Increase the bandwidth to reduce spatial displacement between fat and water signals. |
| Wrap-around artifacts | Activate fold-over suppression to prevent anatomy outside the field of view from overlapping. |
Finally, we will review the images to ensure all the anatomical information we need is clear.
These key structures must be clearly visible in a thoracic spine MRI:
Below, we will go through all the different image contrasts and explain their specific role in imaging the thoracic spine.
T2-weighted imaging makes fluids appear bright. This contrast is ideal for tissues and abnormalities with high water content.
In the thoracic spine, T2 sequences help us view the spinal cord, cerebrospinal fluid (CSF), intervertebral discs, and fluid-related pathologies. Hydrated discs, cysts, or areas of inflammation appear bright, helping us detect conditions like disc degeneration, herniation, and spinal stenosis. T2 also helps us visualize ligaments and assess soft-tissue integrity.
We acquire T2 in coronal, sagittal, and axial views to get complete anatomical coverage. Coronal views show the overall alignment and transverse processes. Sagittal views reveal longitudinal details of the spine and discs. Axial views provide cross-sectional details of the spinal canal and neural structures.
✅ Coronal T2 TSE of Thoracic Spine – Correct Image Example:

Things to Look for in Coronal T2:
✅ Sagittal T2 TSE of Thoracic Spine – Correct Image Example:

Things to Look for in Sagittal T2:
✅ Axial T2 TSE of Thoracic Spine – Correct Image Example:
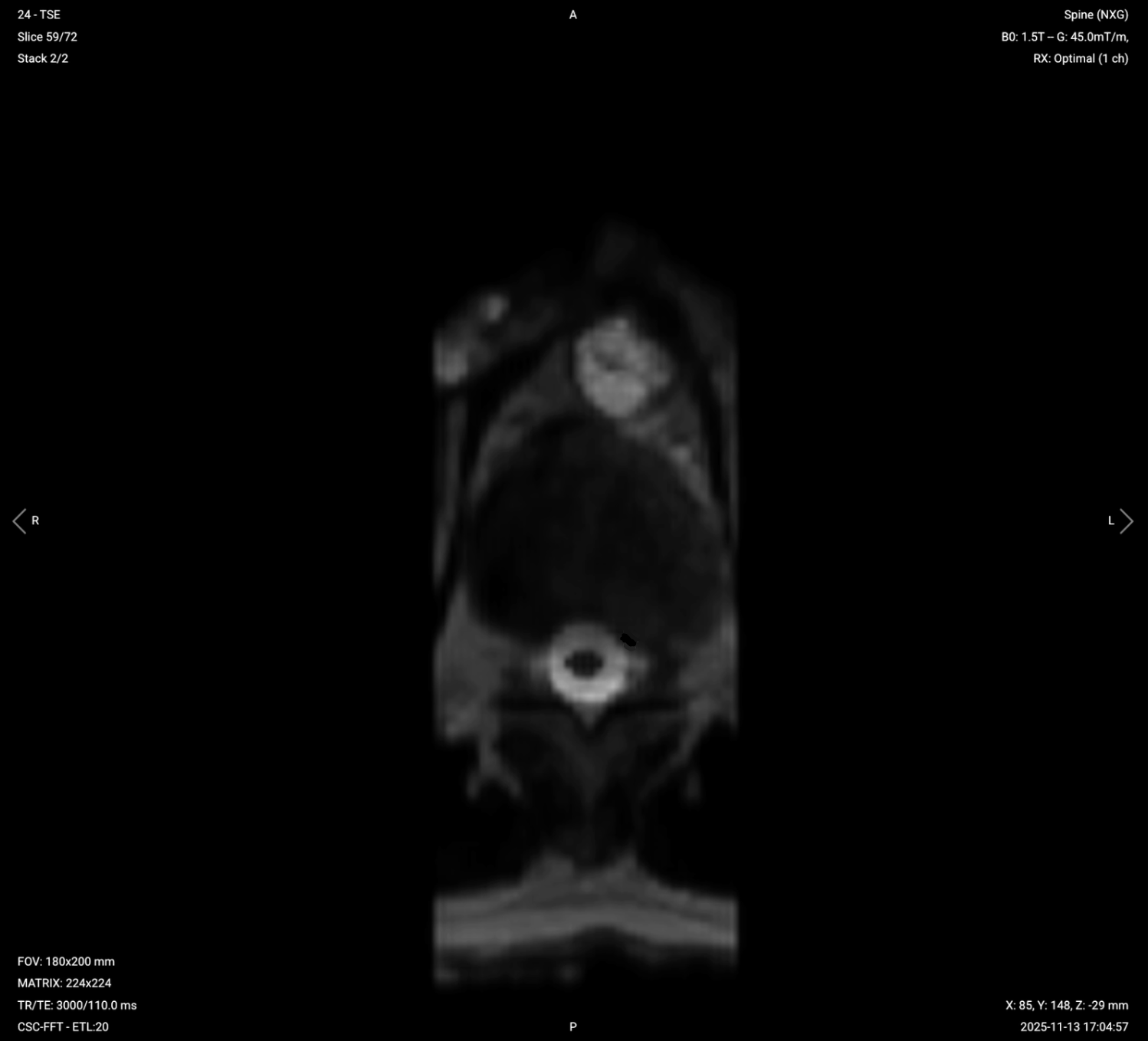
Things to Look for in Axial T2:
T1-weighted imaging makes fat appear bright and fluid dark. This contrast is ideal for fat-rich tissues and structural abnormalities. T1 shows anatomical structures clearly, since it helps us see where different solid tissues like muscle and fat meet.
In the thoracic spine, T1 sequences are ideal for assessing bone marrow, epidural fat, and the integrity of vertebral bodies. Chronic degenerative changes, such as Modic endplate changes, fractures, or tumors, are more apparent with T1 imaging. T1 also provides excellent views of the spinal cord morphology and vertebral body structures.
We acquire T1 in sagittal and axial views. Sagittal views show the overall anatomy, vertebral bodies, and chronic bony changes. Axial views provide detailed cross-sectional anatomy at the level of the spinal canal.
✅ Sagittal T1 TSE of Thoracic Spine – Correct Image Example:

Things to Look for in Sagittal T1:
✅ Axial T1 TSE of Thoracic Spine – Correct Image Example:

Things to Look for in Axial T1:
STIR (Short Tau/TI Inversion Recovery) suppresses fat signals completely, which makes water-rich tissues stand out even clearer than with normal T2 TSE. This makes STIR ideal for detecting subtle fluid-related conditions like edema, inflammation, and infections, where increased water content would otherwise be obscured by fat.
In the thoracic spine, STIR is particularly useful for identifying bone marrow edema, infections like discitis or abscesses, inflammatory processes, and multiple sclerosis plaques. STIR provides high lesion visibility when water content might not be easily visible on standard T2 sequences.
We acquire STIR in the sagittal view to visualize the entire spine and detect any fluid-related changes across vertebrae or discs.
✅ Sagittal STIR TSE of Thoracic Spine – Correct Image Example:

Things to Look for in Sagittal STIR:
Before finishing a thoracic spine MRI, always check these 5 points to ensure diagnostic quality: