
Get FREE Weekly MRI Content

This step-by-step guide is for MRI students, radiographers, and technologists who wish to improve their planning skills and master the shoulder MRI protocol.
What you will learn:
The shoulder contains fine structures like the labrum, rotator cuff tendons, and cartilage that need high resolution to detect subtle tears and pathologies.
We should therefore 1) prioritize resolution, 2) maintain strong SNR for clarity, and 3) optimize scan time as needed.
PD FS sequences offer excellent soft tissue contrast and highlight fluids while suppressing fat signal. This helps us clearly see ligament and tendon tears, labral issues, and bone marrow edema.
Fat suppression avoids interference, so these sequences are ideal for evaluating soft tissues in the shoulder.
| Artifacts | Solution – How to Avoid It |
|---|---|
| Motion artifacts | Shorten the scan time to reduce the risk of patient movement. |
| Magic angle artifacts | Acquire T2-weighted images to check if the signal is artifact or real tendon pathology. |
| Chemical shift artifacts | Increase the bandwidth to reduce spatial shift between fat and water signals. |
| Wrap-around artifacts | Activate fold-over suppression to block signals from anatomy outside the field of view. |
| Susceptibility artifacts | Use spin echo sequences instead of gradient echo sequences. |
| Cross-talk artifacts | Keep enough slice gap to prevent overlap between slices. |
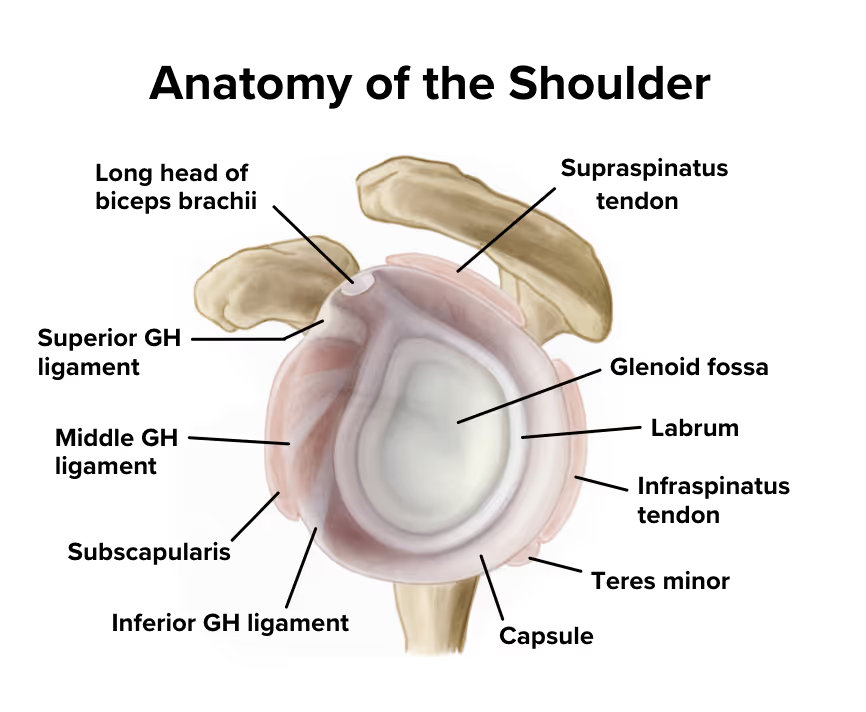
The shoulder is a complex ball-and-socket joint that enables the widest range of motion of any joint in the human body. It consists of multiple structures including the rotator cuff tendons, labrum, joint capsule, and surrounding muscles that work together to provide both mobility and stability.
Because of its complex anatomy and high susceptibility to injuries from sports, repetitive use, and trauma, the shoulder is a frequently examined area in MRI. Imaging helps assess rotator cuff tears, labral damage, impingement syndromes, and other conditions affecting shoulder function and causing pain.
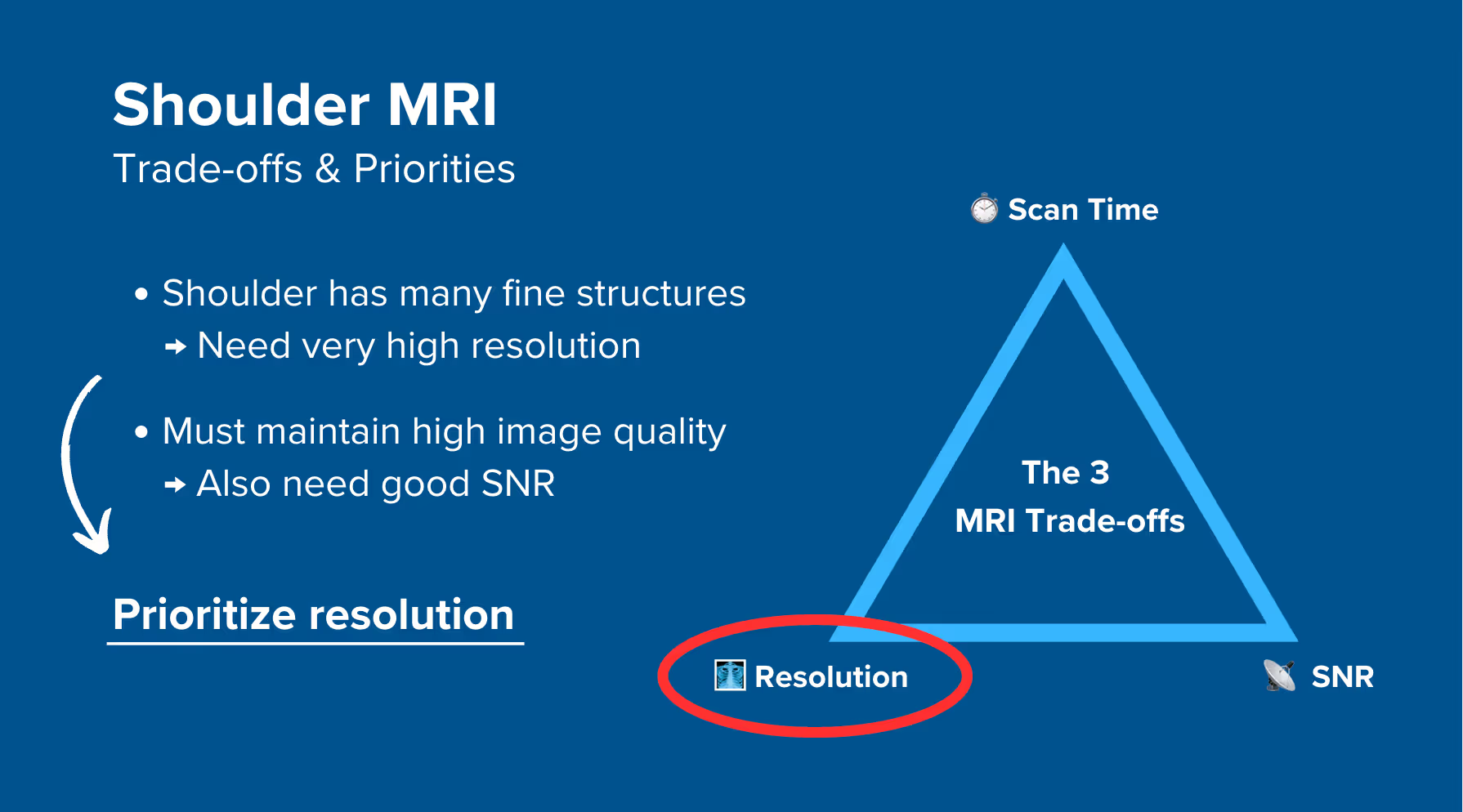
In MRI, we always face a trade-off between 3 key metrics:
Improving one of these metrics reduces the performance of the others. To decide what trade-offs to make, we must consider the needs of each clinical situation.
In shoulder MRIs, we have many fine structures like the labrum, rotator cuff tendons, and cartilage. These require very high resolution to detect subtle tears and pathologies. However, this high resolution reduces SNR, so to maintain image clarity, we must compensate with strong SNR.
Therefore, we typically 1) prioritize resolution, 2) maintain strong SNR for clarity, and 3) optimize scan time as needed for shoulder MRIs.
This ensures we can see small tears and subtle pathologies clearly while maintaining good image quality.
The shoulder MRI study can help us diagnose a wide range of health conditions. The table below lists some of the most common conditions and what pulse sequences reveal them:
| Common Shoulder Conditions | Clearly Seen on Sequence | Why This Sequence? |
|---|---|---|
|
Rotator cuff and labral pathologies: • Rotator cuff tears • Labral tears • SLAP lesions • Tendinopathies • Bursitis |
PD FS (Proton Density Fat-Saturated) | Enhances soft tissues and fluid while suppressing fat signal. Tears appear bright against the dark tendon or labrum. Excellent for detecting tendinosis, partial tears, or inflammation like bursitis. |
|
Structural and bone abnormalities: • Fractures • Avascular necrosis • Hill-Sachs lesions • Fatty infiltration |
T1 TSE | Shows excellent anatomy and highlights fat. Ideal for evaluating bone integrity, chronic marrow changes, and fatty muscle atrophy. Helps confirm chronic structural damage. |
|
Inflammatory and fluid-related conditions: • Bone marrow edema • Joint effusions • Synovitis • Adhesive capsulitis |
T2 TSE | Fluid appears bright, making edema and inflammation easy to spot. Helps diagnose capsular thickening in adhesive capsulitis and confirm tendon pathology by reducing magic angle artifact effects. |
The shoulder joint has complex three-dimensional anatomy, with structures like the labrum, rotator cuff tendons, and joint capsule all packed together. This can make it difficult to describe exactly where issues are located using traditional terms like anterior or superior.
The clock face method solves this communication problem by using the glenoid (the socket of the shoulder) as a clock face when viewed from the side.
With this method:
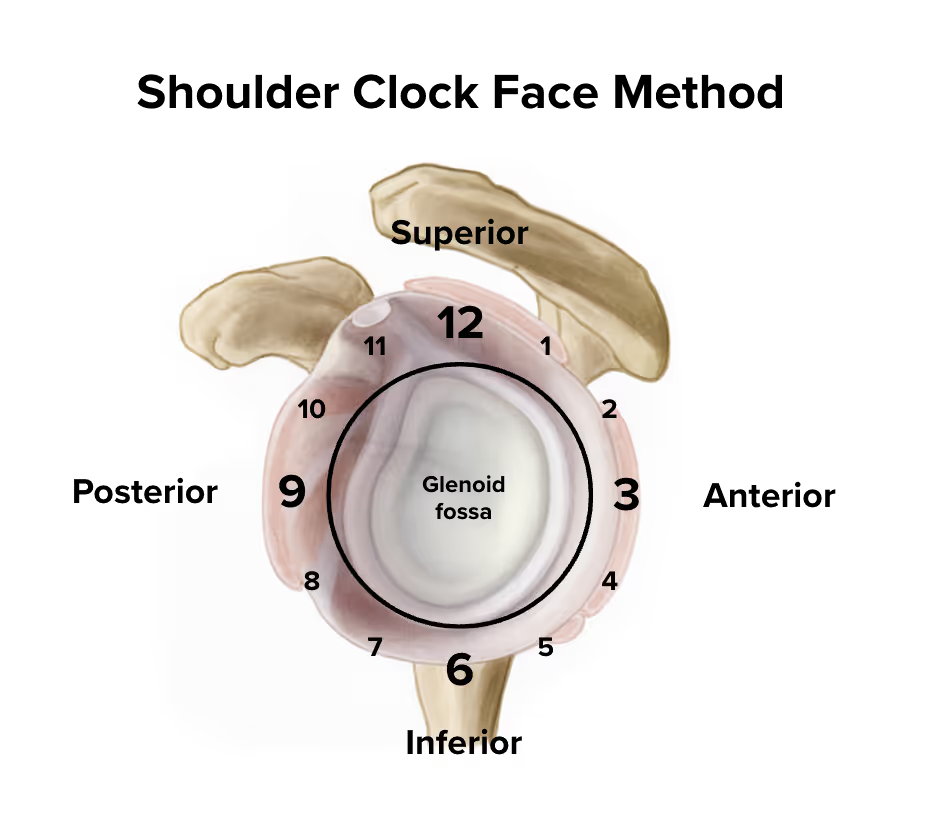
For example, instead of saying a labral tear is in the anterior-superior region, we can say it runs from 1 to 3 o'clock. Or if there's rotator cuff damage, we might say it's located at the 12 o'clock position.
This precision helps surgeons know exactly where to look and what to repair. The clock face method also guides our slice planning to ensure we capture anatomy at the correct angles.
The step-by-step guide below will show you how to set up and perform a shoulder MRI protocol in practice.
We will perform the protocol in 3 parts:
Lay the patient head-first and supine (on their back) with the shoulder aligned at the scanner's isocenter.
Use a dedicated shoulder coil array or flexible coil that surrounds the entire shoulder region to ensure high-resolution imaging. This coil provides strong signal reception and full coverage of the joint, including the rotator cuff, labrum, and surrounding structures.
✅ Correct Patient Positioning:

Once the patient is in place, review your scanner’s hardware settings.
In this guide, we will use the following settings:
| Scanner Setting | Value | Why This Value |
|---|---|---|
| Magnetic field strength | 1.5 T | Enables high Signal-to-Noise Ratio, which gives superior image quality. |
| Maximum gradient strength | 45 mT/m | Enables faster acquisitions while preserving high image quality. |
This hardware setup is widely used in clinical practice. It balances acquisition time, image quality, and patient comfort.
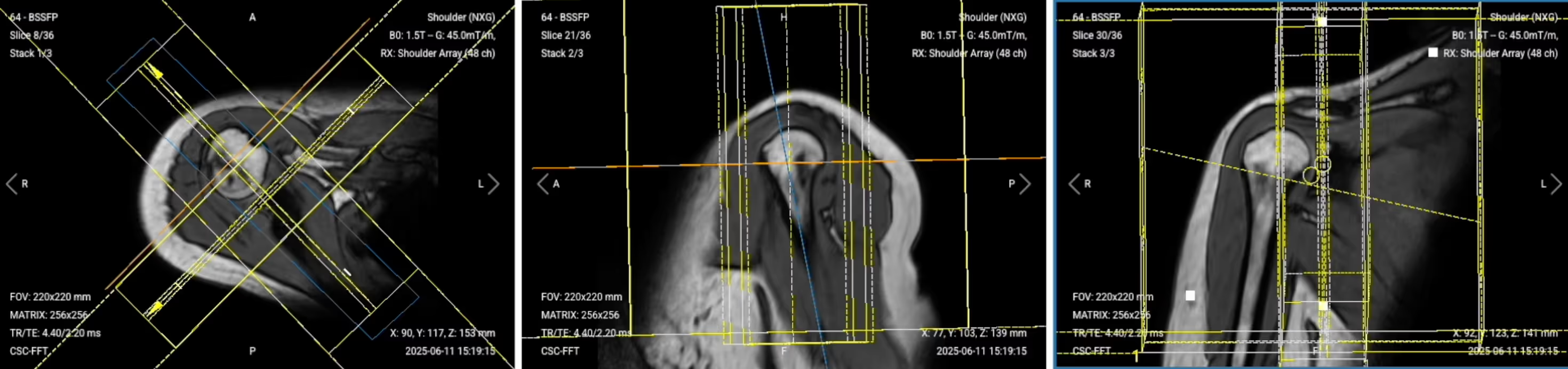
Before we can perform any MRI protocol, we must always capture initial localizer images of the patient. These images act as a guide for planning the detailed scans we will perform next.
We should always capture localizers in three planes:
Once acquired, upload the initial localizer images into the three viewports.
Then, scroll through each of the image stacks to locate a central slice that clearly shows the anatomy of the shoulder.
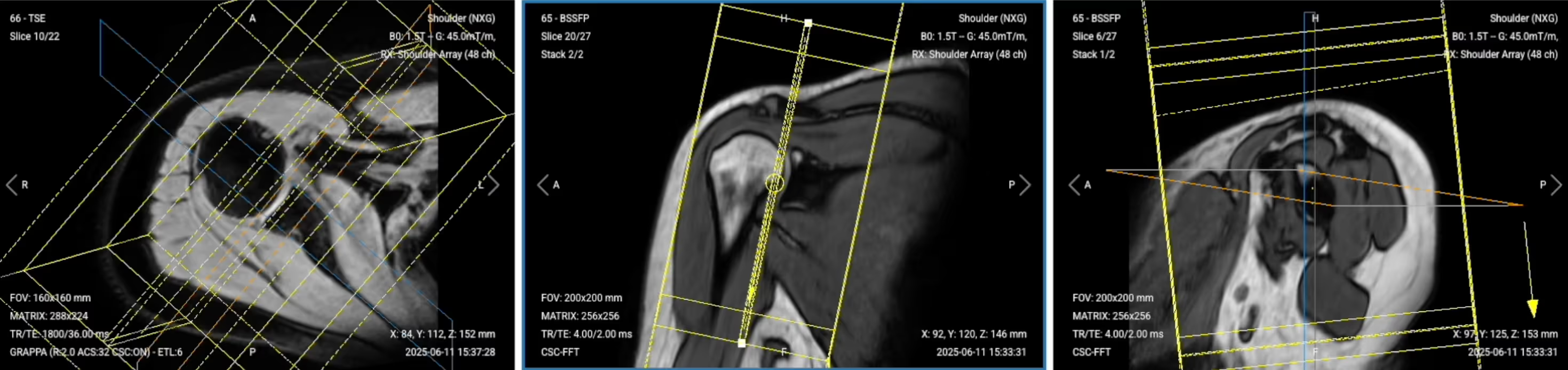
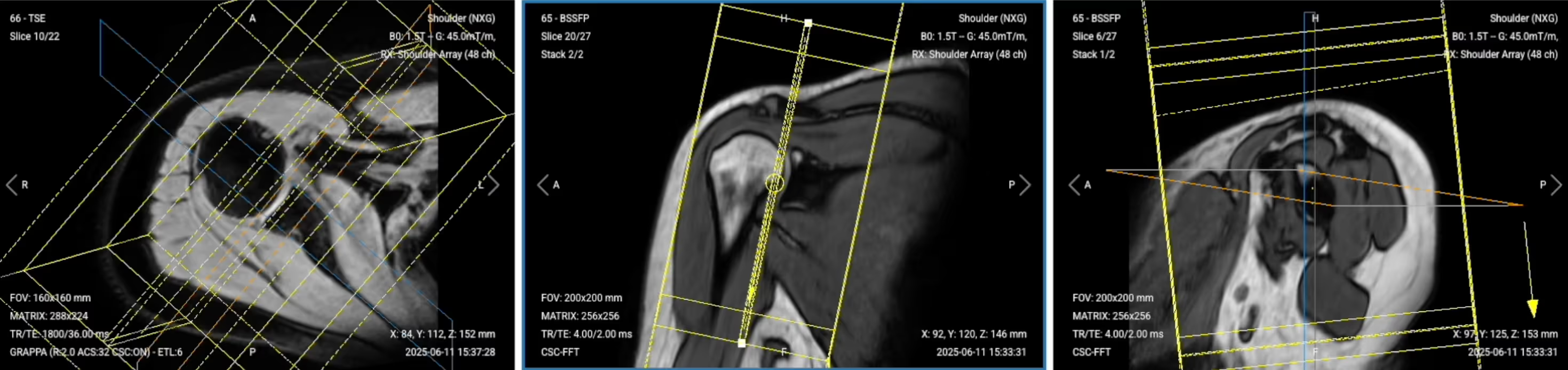
✅ Correct Setup of Localizer Images for Shoulder MRI:

When all preparations are ready, we can start planning and acquiring the protocol sequences.
Let's go through the pulse sequences a standard shoulder MRI protocol includes, why we perform them, and how to set them up.
Before we acquire our high-resolution sequences, we need additional localizers to plan our sequences according to specific anatomical structures using the clock face method.
We’ll run two different localizer sequences:
✅ Correct Planning:
Planning Instructions:
✅ Sagittal Localizer – Correct Image Example:
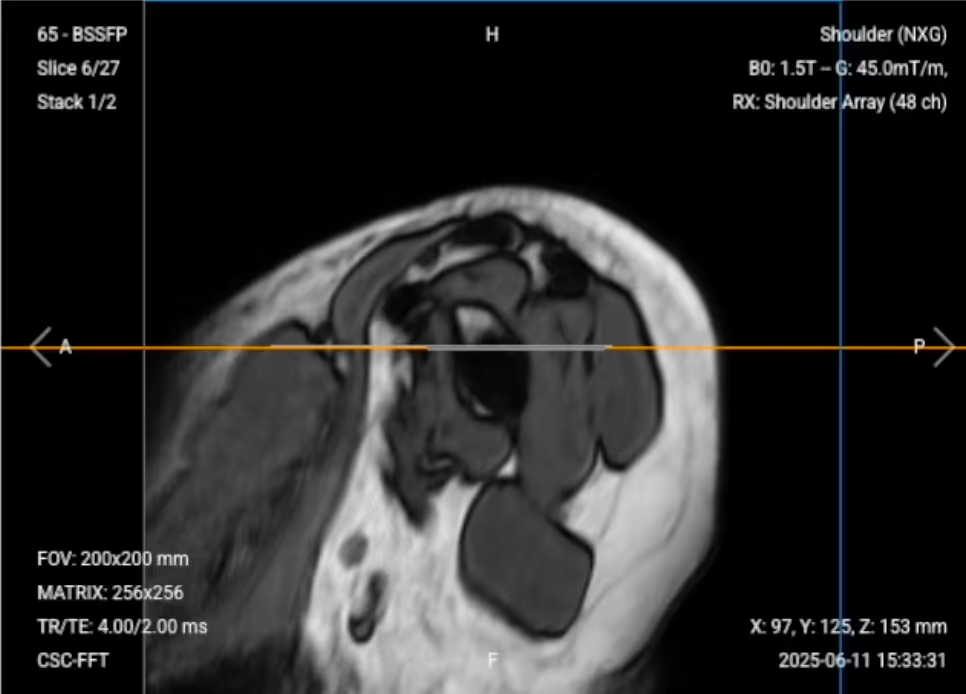
✅ Coronal Localizer – Correct Image Example:
✅ Correct Planning:
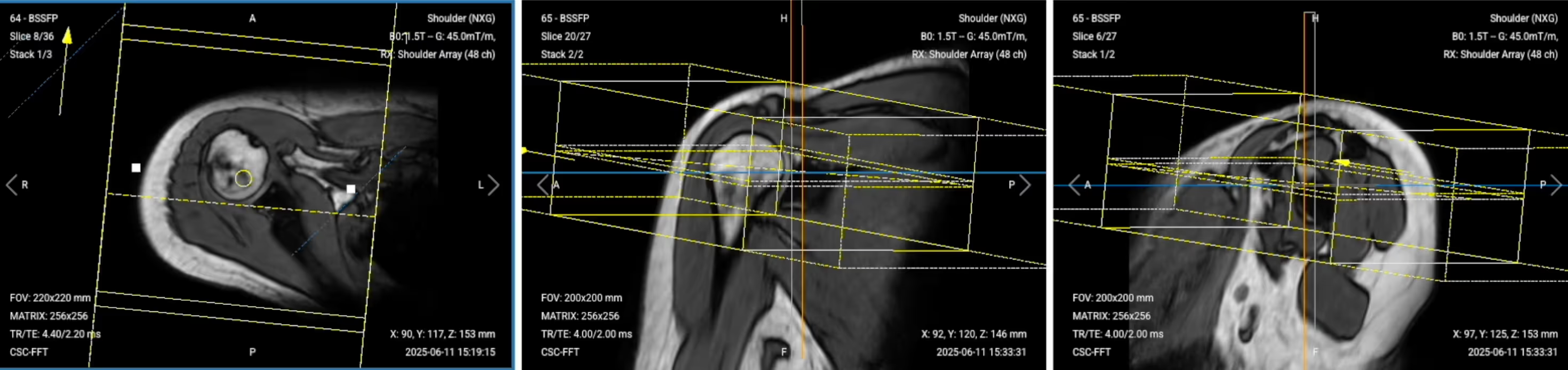
Planning Instructions:
✅ Axial PD Fat-Sat Localizer – Correct Image Example:
Once we have all localizers, we will run the following 6 sequences:
We mainly use Turbo Spin Echo sequences for this study. These sequences let us create multiple types of contrasts, including PD with fat suppression, T1, and T2 weighting. This helps us assess the integrity of the shoulder structures and check for common pathologies while maintaining high resolution for small structures.
The order of sequences is very important for the clock face method. Each sequence helps us plan the next one for optimal visualization of shoulder anatomy.
In the sections below, we go through how to plan and set up each sequence.
✅ Correct Planning:
Planning Instructions:
Parameters for Sagittal PD Fat-Saturated TSE:
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 20–40 ms | Shorter TE is required for PD contrast. |
| Repetition Time (TR) | 1,500–2,500 ms | Longer TR is required for PD contrast. |
| Field-of-View (FOV) | 160 × 160 mm | Small enough to focus on the shoulder region with high resolution. |
| Matrix | 320 × 256 | High matrix size to get excellent resolution for small shoulder structures while maintaining good SNR. |
| Foldover Direction (Phase) | Anterior-to-Posterior (AP) | To reduce motion artifacts and align with natural shoulder orientation. |
| Number of Slices | 25–30 | Enough slices to cover from deltoid muscle to scapular notch. |
| Slice Thickness | 3 mm | Thin enough for high resolution without sacrificing scan time or SNR. |
| Slice Gap | 0.3 mm | 10% of slice thickness to enhance small structure visibility and maintain continuity. |
| NEX / Averages | 1–2 | To get enough SNR while keeping scan time reasonable. |
| Turbo Factor / ETL | 6 | Lower turbo factor to minimize T2-weighting and get purer PD contrast. |
| Bandwidth | 100,000 Hz | High enough to avoid chemical shift artifacts without reducing SNR. |
| Fold-over Suppression | Yes | To avoid aliasing or wrap-around artifacts. |
| Fat Suppression | Spectral | To nullify fat signal and make soft tissues, tendons, and fluid-related abnormalities more visible. |
✅ Correct Planning:

Planning Instructions:
Parameters for Coronal PD Fat-Saturated TSE:
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 20–40 ms | Shorter TE is required for PD contrast. |
| Repetition Time (TR) | 1,500–2,500 ms | Longer TR is required for PD contrast. |
| Field-of-View (FOV) | 160 × 160 mm | Small enough to focus on the shoulder region with high resolution. |
| Matrix | 320 × 256 | High matrix size to get excellent resolution for small shoulder structures while maintaining good SNR. |
| Foldover Direction (Phase) | Anterior-to-Posterior (AP) | To reduce motion artifacts and align with natural shoulder orientation. |
| Number of Slices | 25–30 | Enough slices to cover from coracoid process to behind humeral head. |
| Slice Thickness | 3 mm | Thin enough for high resolution without sacrificing scan time or SNR. |
| Slice Gap | 0.3 mm | 10% of slice thickness to enhance small structure visibility and maintain continuity. |
| NEX / Averages | 1–2 | To get enough SNR while keeping scan time reasonable. |
| Turbo Factor / ETL | 6 | Lower turbo factor to minimize T2-weighting and get purer PD contrast. |
| Bandwidth | 100,000 Hz | High enough to avoid chemical shift artifacts without reducing SNR. |
| Fold-over Suppression | Yes | To avoid aliasing or wrap-around artifacts. |
| Fat Suppression | Spectral | To nullify fat signal and make soft tissues, tendons, and fluid-related abnormalities more visible. |
✅ Correct Planning:
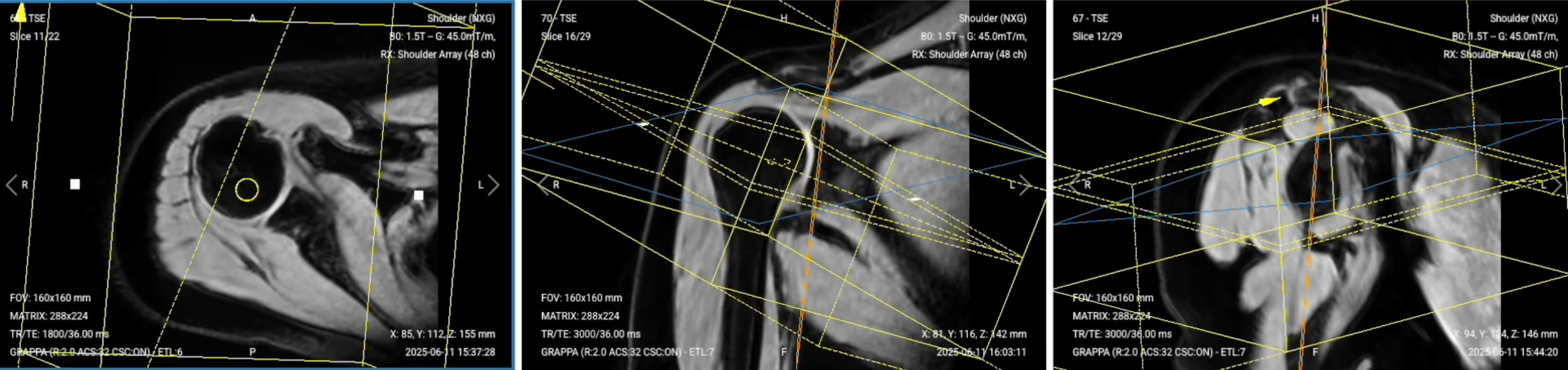
Planning Instructions:
Parameters for Axial PD Fat-Saturated TSE:
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 20–40 ms | Shorter TE is required for PD contrast. |
| Repetition Time (TR) | 1,500–2,500 ms | Longer TR is required for PD contrast. |
| Field-of-View (FOV) | 160 × 160 mm | Small enough to focus on the shoulder region with high resolution. |
| Matrix | 320 × 256 | High matrix size to get excellent resolution for small shoulder structures while maintaining good SNR. |
| Foldover Direction (Phase) | Anterior-to-Posterior (AP) | To reduce motion artifacts and align with natural shoulder orientation. |
| Number of Slices | 25–30 | Enough slices to cover from acromioclavicular joint to below articular capsule. |
| Slice Thickness | 3 mm | Thin enough for high resolution without sacrificing scan time or SNR. |
| Slice Gap | 0.3 mm | 10% of slice thickness to enhance small structure visibility and maintain continuity. |
| NEX / Averages | 1–2 | To get enough SNR while keeping scan time reasonable. |
| Turbo Factor / ETL | 6 | Lower turbo factor to minimize T2-weighting and get purer PD contrast. |
| Bandwidth | 100,000 Hz | High enough to avoid chemical shift artifacts without reducing SNR. |
| Fold-over Suppression | Yes | To avoid aliasing or wrap-around artifacts. |
| Fat Suppression | Spectral | To nullify fat signal and make soft tissues, tendons, and fluid-related abnormalities more visible. |
✅ Correct Planning:
Planning Instructions:
Parameters for Sagittal T1 TSE:
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 10 ms | Shorter TE is required for T1 contrast. |
| Repetition Time (TR) | 400 ms | Shorter TR is required for T1 contrast. |
| Field-of-View (FOV) | 160 × 160 mm | Small enough to focus on the shoulder region with high resolution. |
| Matrix | 320 × 256 | High matrix size to get excellent resolution for small shoulder structures while maintaining good SNR. |
| Foldover Direction (Phase) | Anterior-to-Posterior (AP) | To reduce motion artifacts and align with natural shoulder orientation. |
| Number of Slices | 29 | Enough slices to cover from deltoid muscle to scapular notch. |
| Slice Thickness | 3 mm | Thin enough for high resolution without sacrificing scan time or SNR. |
| Slice Gap | 0.3 mm | 10% of slice thickness to enhance small structure visibility and maintain continuity. |
| NEX / Averages | 1–2 | To get enough SNR while keeping scan time reasonable. |
| Turbo Factor / ETL | 2 | Lower turbo factor for T1 contrast to minimize T2-weighting. |
| Bandwidth | 100,000 Hz | High enough to avoid chemical shift artifacts without reducing SNR. |
| Fold-over Suppression | Yes | To avoid aliasing or wrap-around artifacts. |
| Fat Suppression | None | Not needed for T1 sequences. |
✅ Correct Planning:

Planning Instructions:
Parameters for Coronal T2 TSE:
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 30 ms | Moderate TE for T2 contrast while avoiding magic angle artifacts. |
| Repetition Time (TR) | 3,000 ms | Longer TR is required for T2 contrast. |
| Field-of-View (FOV) | 160 × 160 mm | Small enough to focus on the shoulder region with high resolution. |
| Matrix | 320 × 256 | High matrix size to get excellent resolution for small shoulder structures while maintaining good SNR. |
| Foldover Direction (Phase) | Anterior-to-Posterior (AP) | To reduce motion artifacts and align with natural shoulder orientation. |
| Number of Slices | 25–30 | Enough slices to cover from coracoid process to behind humeral head. |
| Slice Thickness | 3 mm | Thin enough for high resolution without sacrificing scan time or SNR. |
| Slice Gap | 0.3 mm | 10% of slice thickness to enhance small structure visibility and maintain continuity. |
| NEX / Averages | 1–2 | To get enough SNR while keeping scan time reasonable. |
| Turbo Factor / ETL | 12 | Higher turbo factor to enhance T2 contrast and optimize scan time. |
| Bandwidth | 100,000 Hz | High enough to avoid chemical shift artifacts without reducing SNR. |
| Fold-over Suppression | Yes | To avoid aliasing or wrap-around artifacts. |
| Fat Suppression | None | Not typically used for T2 sequences in shoulder imaging. |
✅ Correct Planning:
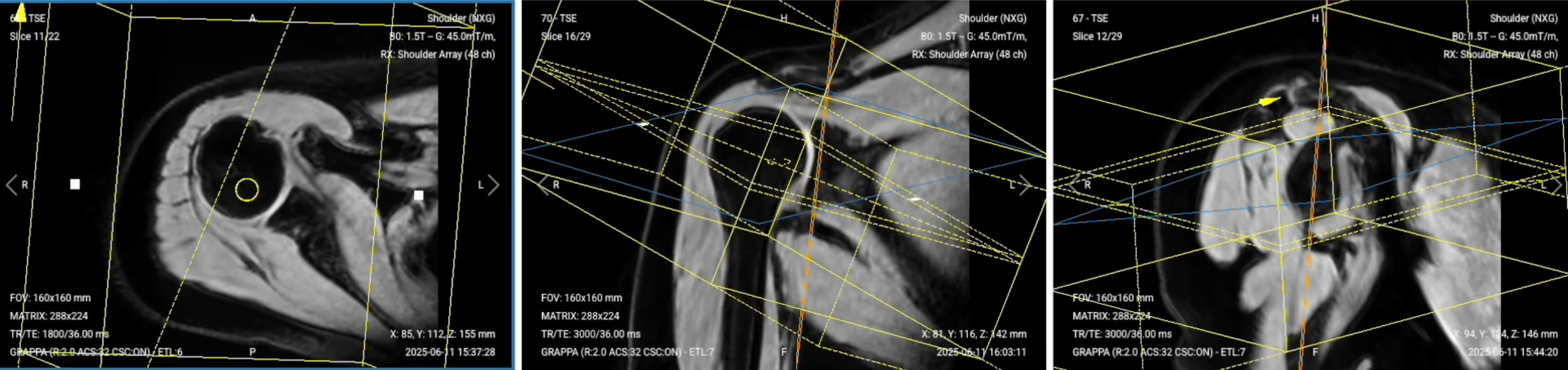
Planning Instructions:
Parameters for Axial T1 TSE:
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 10 ms | Shorter TE is required for T1 contrast. |
| Repetition Time (TR) | 400 ms | Shorter TR is required for T1 contrast. |
| Field-of-View (FOV) | 160 × 160 mm | Small enough to focus on the shoulder region with high resolution. |
| Matrix | 320 × 256 | High matrix size to get excellent resolution for small shoulder structures while maintaining good SNR. |
| Foldover Direction (Phase) | Anterior-to-Posterior (AP) | To reduce motion artifacts and align with natural shoulder orientation. |
| Number of Slices | 25–30 | Enough slices to cover from acromioclavicular joint to below articular capsule. |
| Slice Thickness | 3 mm | Thin enough for high resolution without sacrificing scan time or SNR. |
| Slice Gap | 0.3 mm | 10% of slice thickness to enhance small structure visibility and maintain continuity. |
| NEX / Averages | 1–2 | To get enough SNR while keeping scan time reasonable. |
| Turbo Factor / ETL | 2 | Lower turbo factor for T1 contrast to minimize T2-weighting. |
| Bandwidth | 100,000 Hz | High enough to avoid chemical shift artifacts without reducing SNR. |
| Fold-over Suppression | Yes | To avoid aliasing or wrap-around artifacts. |
| Fat Suppression | None | Not needed for T1 sequences. |
The table below lists the 5 common shoulder artifacts, and what techniques you can use to avoid them:
| Artifacts | Solution – How to Avoid It |
|---|---|
| Motion artifacts | Shorten the scan time to reduce the risk of patient movement. |
| Magic angle artifacts | Acquire T2-weighted images to check if the signal is artifact or real tendon pathology. |
| Chemical shift artifacts | Increase the bandwidth to reduce spatial shift between fat and water signals. |
| Wrap-around artifacts | Activate fold-over suppression to block signals from anatomy outside the field of view. |
| Susceptibility artifacts | Use spin echo sequences instead of gradient echo sequences. |
| Cross-talk artifacts | Keep enough slice gap to prevent overlap between slices. |
Finally, we will review the images to ensure all the anatomical information we need is clear.
These key structures must be clearly visible in a shoulder MRI:
Below, we will go through all the different image contrasts and explain their specific role in imaging the shoulder.
Proton Density Fat-Saturated (PD FS) imaging provides excellent soft tissue contrast while suppressing fat, making it ideal for evaluating shoulder joint structures.
In shoulder MRI, PD FS sequences are the gold standard for detecting rotator cuff tears, labral injuries, and joint effusions. They enhance soft tissues and fluids without fat signal interference, making tears appear as bright signal that interrupts the normally dark tendon or labrum. This contrast is optimal for detecting subtle tendinosis and capsular pathologies.
The three planes captured in PD FS provide comprehensive coverage. Each plane helps plan the next using the clock face method, ensuring optimal visualization of all shoulder structures.
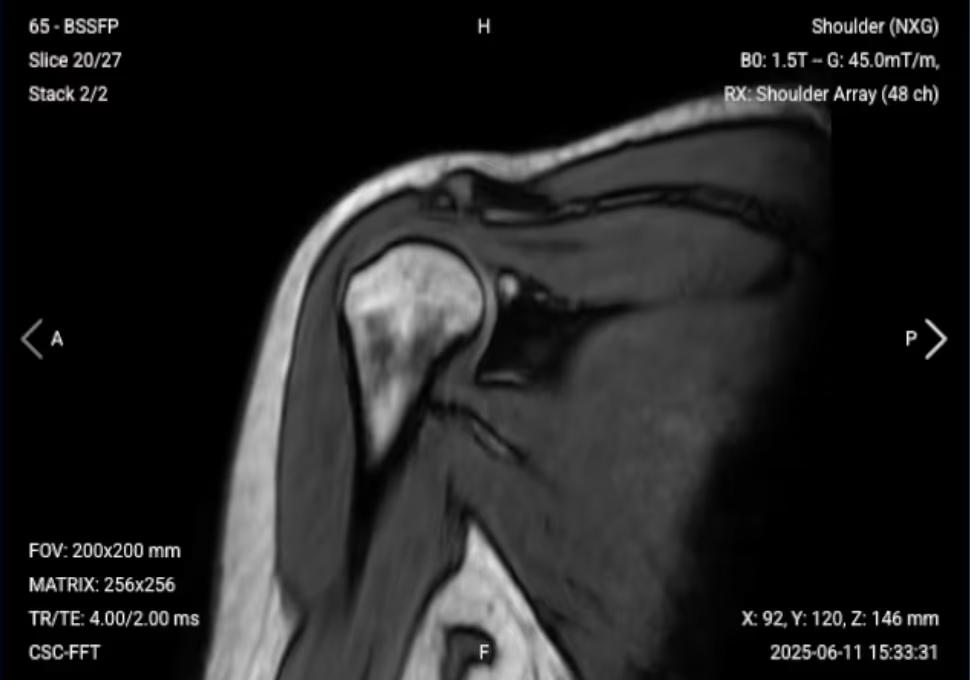
✅ Sagittal PD FS of the Shoulder – Correct Image Example:

Things to Look for in Sagittal PD FS:
✅ Coronal PD FS of the Shoulder – Correct Image Example:

Things to Look for in Coronal PD FS:
✅ Axial PD FS of the Shoulder – Correct Image Example:

Things to Look for in Axial PD FS:
T1-weighted imaging makes fat appear bright and fluid dark. This contrast is ideal for fat-rich tissues and structural abnormalities. T1 shows anatomical structures clearly since it helps us see where different solid tissues like muscle and fat meet.
In shoulder MRI, T1 sequences are valuable for evaluating bone marrow pathology, fatty infiltration of muscles, and overall anatomical structure. T1 contrast helps identify bone marrow changes, muscle atrophy, and provides baseline anatomy for comparison with other sequences
✅ Sagittal T1 of the Shoulder – Correct Image Example:

Things to Look for in Sagittal T1:
✅ Axial T1 of the Shoulder – Correct Image Example:

Things to Look for in Axial T1:
T2-weighted imaging makes fluids appear bright. This contrast is ideal for detecting tissues and abnormalities with high water content.
In shoulder MRI, T2 sequences help confirm pathology seen on other sequences and distinguish real inflammation from magic angle artifacts. They are particularly useful for evaluating edema, inflammation, joint effusions, and confirming whether increased signal on other sequences represents true pathology.
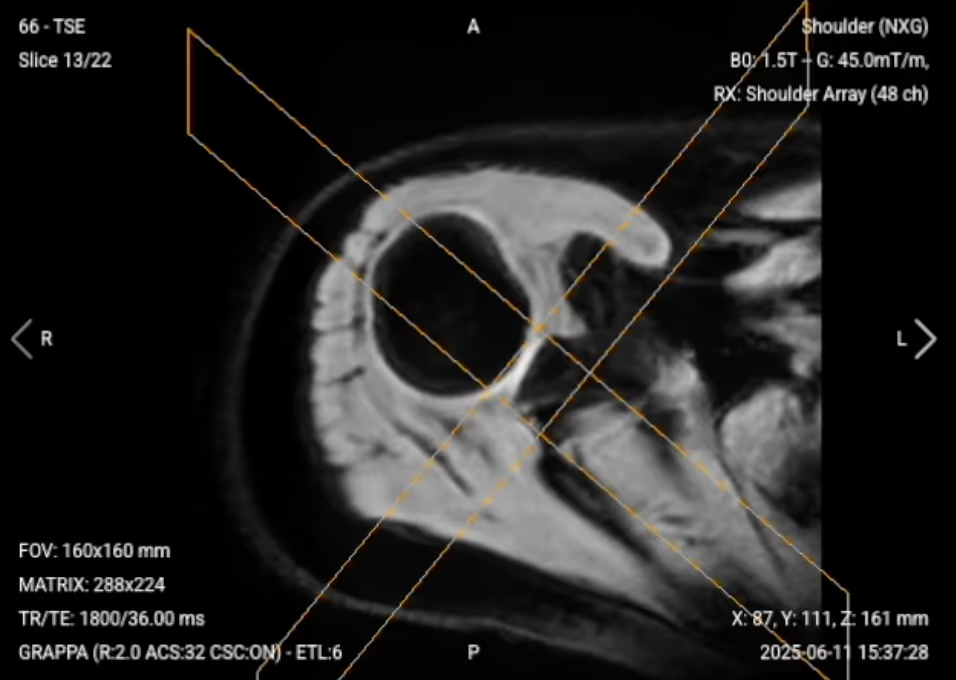
✅ Coronal T2 of the Shoulder – Correct Image Example:

Things to Look for in Coronal T2:
Before finishing a shoulder MRI, always check these 5 points to ensure diagnostic quality: