
Get FREE Weekly MRI Content

This step-by-step guide is for MRI students, radiographers, and technologists who wish to improve their planning skills and master the anal fistula MRI protocol.
What you will learn:
The anal canal has complex, small structures where fistulas can form branching patterns. We need high resolution to detect these subtle tracts while keeping scan time short to avoid motion artifacts.
We typically 1) prioritize resolution, 2) maintain short scan time, and 3) optimize SNR as needed.
T2 sequences make fluid appear bright, helping us see fistula tracts clearly against darker tissue. Fat saturation enhances this contrast by suppressing the bright fat signal.
This makes inflamed tissue and fluid collections stand out more.
| Artifacts | Solution – How to Avoid It |
|---|---|
| Motion artifacts | Shorten scan time using parallel imaging or radial k-space acquisition (BLADE/PROPELLER). |
| Susceptibility artifacts | Use turbo spin echo instead of gradient echo sequences to reduce sensitivity to gas interfaces. |
| Wrap-around artifacts | Activate fold-over suppression to prevent anatomy outside the field of view from overlapping. |
| Chemical shift artifacts | Increase the bandwidth to reduce the spatial displacement between fat and water signals. |
| Fat suppression failure | Use STIR instead of spectral fat saturation when field inhomogeneity is present. |
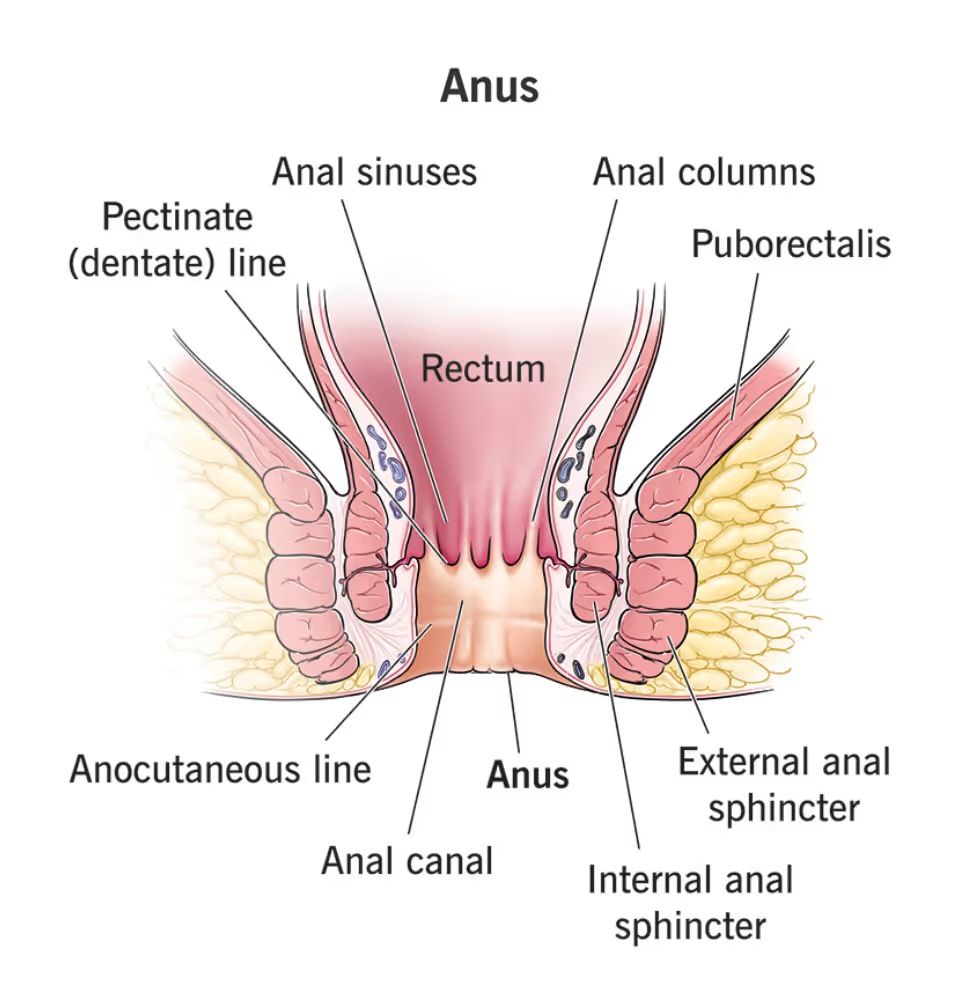
The anal canal and surrounding perianal region are complex anatomical areas where abnormal connections called fistulas can develop between the anal canal and the skin surface. These tracts often result from infection, inflammation, or surgical complications.
Anal fistula MRI is one of the most important pelvic imaging protocols for colorectal surgery planning. It provides detailed visualization of fistula tracts, their relationship to sphincter muscles, and any associated abscesses or inflammation.
In MRI, we always face a trade-off between 3 key metrics:
Improving one of these metrics reduces the performance of the others. To decide what trade-offs to make, we must consider the needs of each clinical situation.
In anal fistula MRIs, we need to visualize tiny fluid-filled tracts in soft tissue. The pelvic region is also subject to bowel movement and other motion. Small or branching fistulas require exceptional detail to plan surgery properly.
Therefore, we typically 1) prioritize resolution, 2) maintain short scan time to reduce motion artifacts, and 3) optimize SNR as needed for clear tissue contrast.

The anal fistula MRI study helps us diagnose and characterize various perianal conditions. The table below lists the most common conditions and the pulse sequences that reveal them:
| Common Anal Fistula Conditions | Clearly Seen on Sequence | Why This Sequence? |
|---|---|---|
|
Fistula tracts and classification: • Intersphincteric fistulas • Transsphincteric fistulas • Horseshoe fistulas |
T2 TSE | Makes fluid appear bright against darker tissue, clearly showing tubular fistula tracts. Simple fistulas run straight from internal to external sphincter, while complex ones branch or take indirect paths. |
|
Inflammatory collections: • Perianal abscesses • Perirectal abscesses • Fluid collections |
T2 TSE Fat-Saturated | Suppresses fat to highlight fluid collections and inflamed tissue. The increased contrast-to-noise ratio between normal fat and abnormal fluid makes even small abscesses visible. Critical for identifying hidden pockets of infection. |
|
Fluid and edema detection: • Edema • Cellulitis • Inflammatory fluid |
T2 STIR TSE | Nulls fat signal completely while highlighting all water content in tissues. Shows the full extent of edema and inflammatory spread. Detects inflammation based on increased water content, whether acute or chronic. Most sensitive for mapping inflammatory extent. |
|
Structural abnormalities: • Postoperative changes • Scar tissue • Chronic fibrosis |
T1 TSE (Pre-contrast) |
Highlights fat and provides clear anatomical contrast. Shows structural details and chronic changes. Provides baseline anatomy before contrast administration. |
|
Active disease and viability: • Abscess walls (rim enhancement) • Active granulation tissue • Tumor involvement • Fistula tract viability |
T1 TSE (Post-contrast) |
Shows tissues with active blood supply through enhancement. Granulation tissue enhances, fibrosis does not. Abscess walls show rim enhancement. Critical for differentiating healing tissue from scar. |
The step-by-step guide below will show you how to set up and perform an anal fistula MRI protocol in practice.
We will perform the protocol in 3 parts:
Before scanning, proper patient preparation is crucial for optimal image quality.
The patient should empty their bladder before the exam. A full bladder can deform rectal anatomy and create interfaces between fluid and gas that impair fat suppression.
Ask the patient to avoid gas-producing foods like fiber for 24 hours before the scan if possible. Excessive bowel gas creates susceptibility artifacts and degrades image quality.
Some protocols may require a small rectal enema to clear feces from the rectum, but this is institution-specific.
Lay the patient feet-first and supine (on their back) with the pelvis centered at the scanner's isocenter.
Using a feet-first position makes the scan feel less claustrophobic for the patient, which reduces the risk of motion artifacts.
Use a pelvic phased-array coil or body coil to ensure high-resolution imaging. Position the coil's upper border at the iliac crest. This coil provides strong signal reception and full coverage of the perianal region.
✅ Correct Patient Positioning:

Once the patient is in place, review your scanner’s hardware settings.
In this guide, we will use the following settings:
| Scanner Setting | Value | Why This Value |
|---|---|---|
| Magnetic field strength | 1.5 T | Enables high Signal-to-Noise Ratio, which gives superior image quality. |
| Maximum gradient strength | 45 mT/m | Enables faster acquisitions while preserving high image quality. |
This hardware setup is widely used in clinical practice. It balances acquisition time, image quality, and patient comfort.
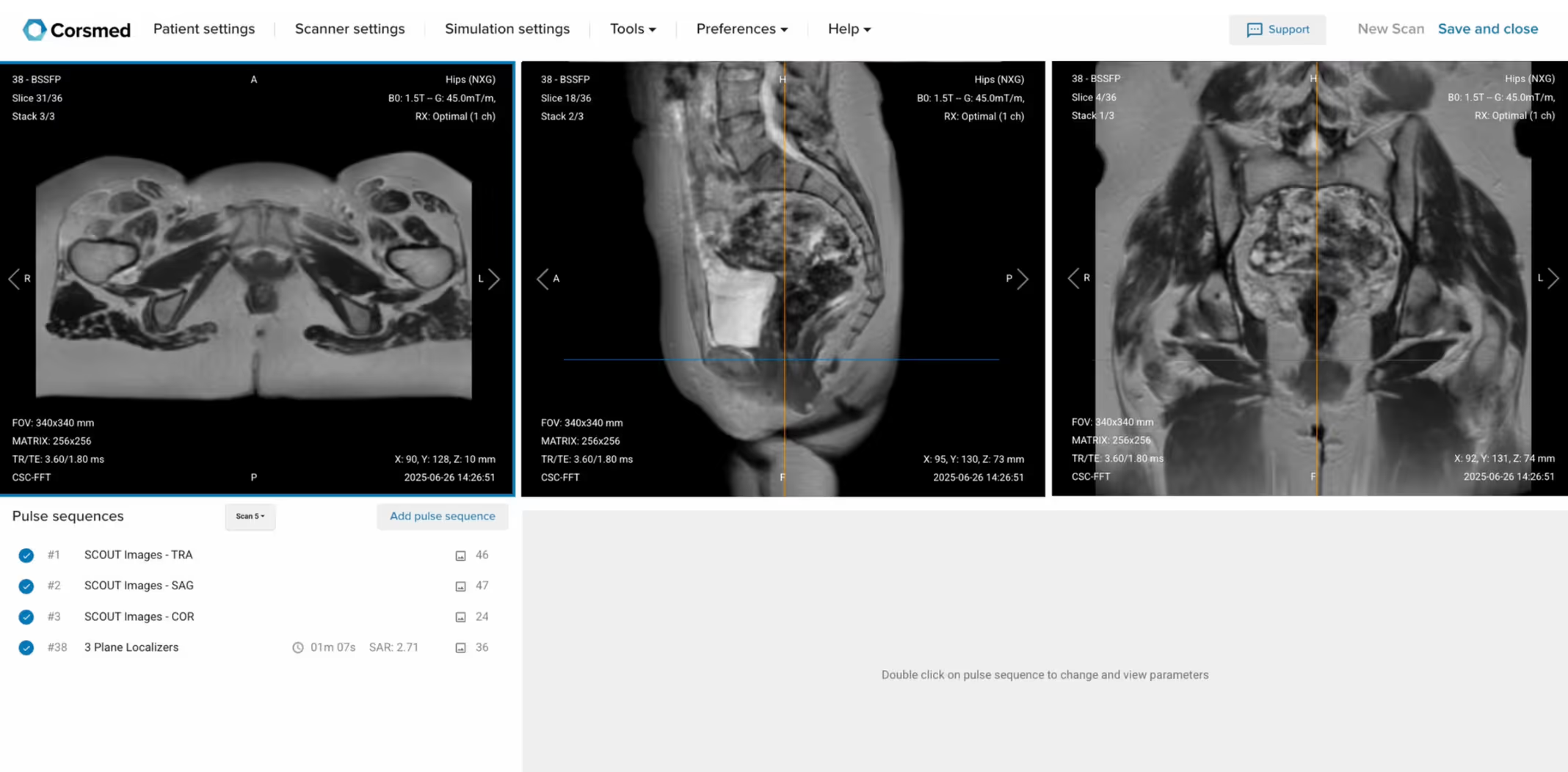
Before we can perform any MRI protocol, we must always capture initial localizer images of the patient. These images act as a guide for planning the detailed scans we will perform next.
We should always capture localizers in three planes:
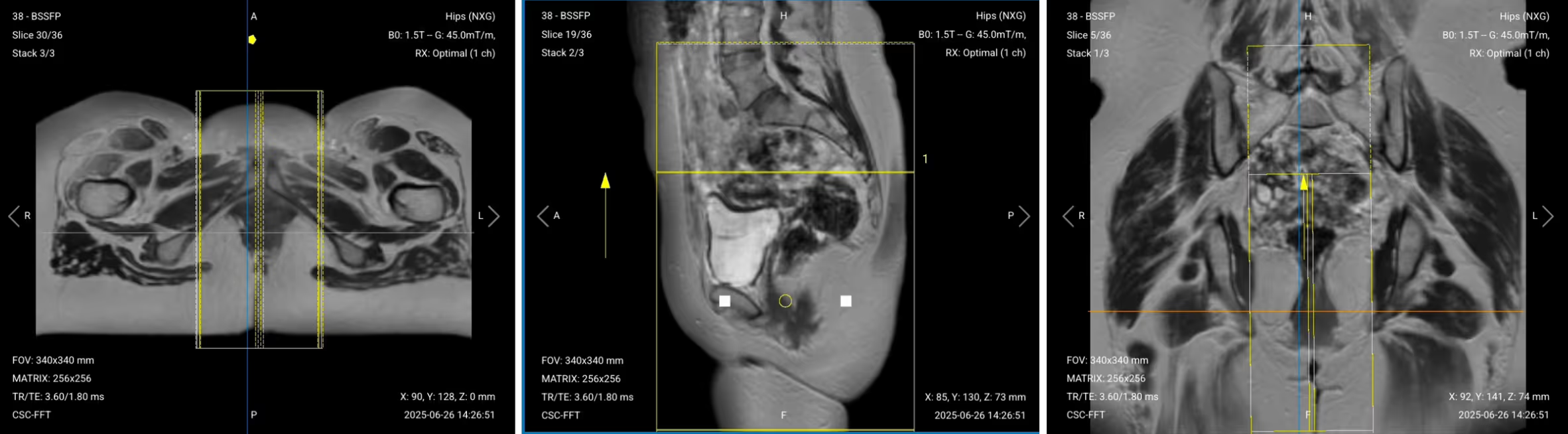
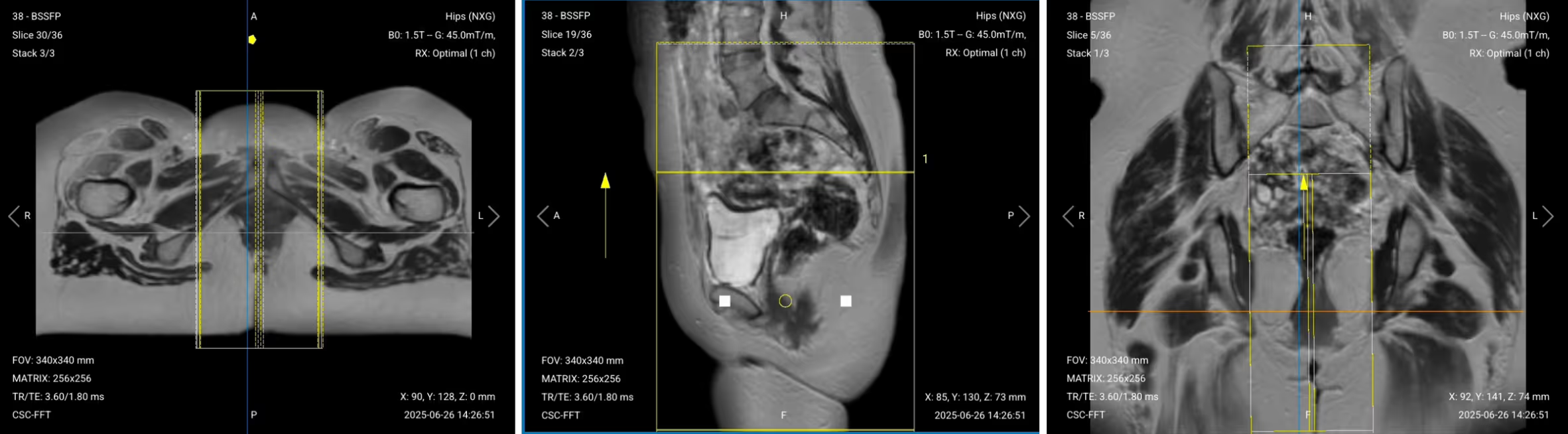
Once acquired, upload the initial localizer images into the three viewports.
Then, scroll through each of the image stacks to locate a central slice that clearly shows the anatomy of the anal canal.
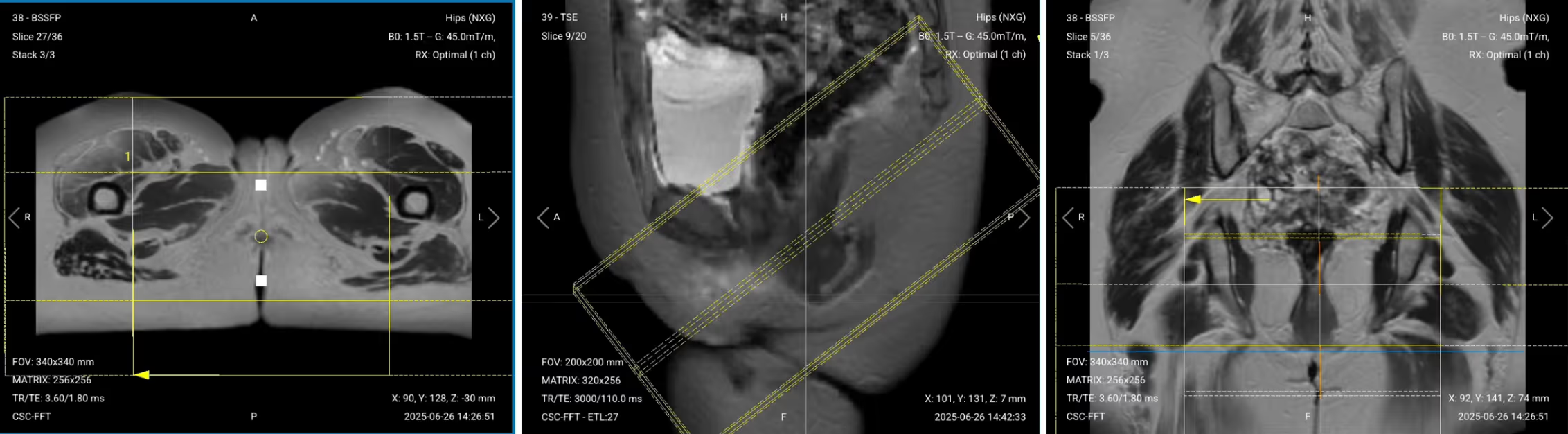
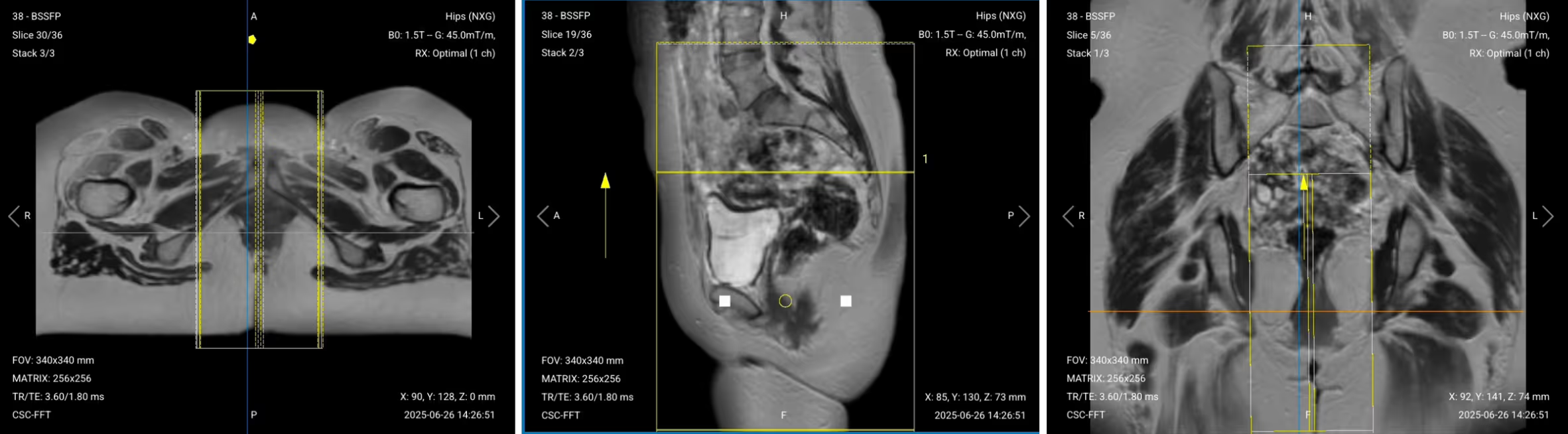
✅ Correct Setup of Localizer Images for Anal Fistula MRI:
When all preparations are ready, we can start planning and acquiring the protocol sequences.
Let's go through the pulse sequences a standard anal fistula MRI protocol includes, why we perform them, and how to set them up.
We mainly use T2 Turbo Spin Echo sequences with fat saturation for this study. These sequences make fluid appear bright, which helps us detect fistula tracts, abscesses, and inflammation clearly against darker tissue.
Fat saturation techniques enhance this contrast further by suppressing the bright fat signal. This increases the contrast-to-noise ratio between pathology and normal tissue.
In the sections below, we go through how to plan and set up each sequence.
✅ Correct Planning:
Planning Instructions:
Parameters for Sagittal T2 TSE High Resolution:
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 90–110 ms | Longer TE required for T2 contrast to highlight fluid. |
| Repetition Time (TR) | 3,000–4,000 ms | Longer TR required for T2 contrast. |
| Field-of-View (FOV) | 200 × 200 mm | Small enough to focus on the perianal region with high detail. |
| Matrix | 320 × 320 | High matrix for excellent resolution to detect small fistula tracts. |
| Foldover Direction (Phase) | Foot-to-Head (FH) | Reduces respiratory motion and wrap artifacts. |
| Number of Slices | 15–20 | Enough to cover the entire perianal region and lower rectum. |
| Slice Thickness | 3 mm | Thin slices for high resolution without losing too much SNR. |
| Slice Gap | 0.3 mm | Minimal gap (10% of thickness) prevents crosstalk while maintaining continuity. |
| NEX / Averages | 2 | Higher averages improve SNR for better visualization of small structures. |
| Turbo Factor / ETL | 15–18 | High turbo factor for faster scanning while maintaining T2 contrast. |
| Bandwidth | 150–200 Hz/px | Medium bandwidth balances chemical shift reduction with SNR preservation. |
| Fold-over Suppression | Yes | Prevents wrap-around artifacts from adjacent anatomy. |
The following T2 sequences will use fat suppression.
When imaging anal fistulas, however, it’s very important to select the right fat suppression technique for image quality.
There are two main fat suppression options:
Which to Choose for Anal Fistula MRI:
The typical inversion time for STIR at 1.5T is 150-180 milliseconds. While STIR takes longer than SPAIR, its robust suppression often makes it worth the extra time in pelvic imaging.
✅ Correct Planning:
Planning Instructions:
Parameters for Sagittal T2 TSE Fat-Saturated:
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 90–110 ms | Longer TE required for T2 contrast to highlight fluid. |
| Repetition Time (TR) | 3,000–4,000 ms | Longer TR required for T2 contrast. |
| Inversion Time (TI) | 150–180 ms (for STIR) | Nulls fat signal at 1.5T for robust suppression. |
| Field-of-View (FOV) | 200 × 200 mm | Small enough to focus on the perianal region with high detail. |
| Matrix | 320 × 320 | High matrix for excellent resolution to detect small fistula tracts. |
| Foldover Direction (Phase) | Foot-to-Head (FH) | Reduces respiratory motion and wrap artifacts. |
| Number of Slices | 15–20 | Enough to cover the entire perianal region and lower rectum. |
| Slice Thickness | 3 mm | Thin slices for high resolution without losing too much SNR. |
| Slice Gap | 0.3 mm | Minimal gap (10% of thickness) prevents crosstalk while maintaining continuity. |
| NEX / Averages | 2 | Higher averages improve SNR for better visualization of small structures. |
| Turbo Factor / ETL | 15–18 | High turbo factor for faster scanning while maintaining T2 contrast. |
| Bandwidth | 150–200 Hz/px | Medium bandwidth balances chemical shift reduction with SNR preservation. |
| Fat Suppression | STIR or SPAIR | STIR more robust for inhomogeneous fields; SPAIR faster if field is uniform. |
| Fold-over Suppression | Yes | Prevents wrap-around artifacts from adjacent anatomy. |
✅ Correct Planning:
Planning Instructions:
Parameters for Axial T2 TSE Fat-Saturated:
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 90–110 ms | Longer TE required for T2 contrast to highlight fluid. |
| Repetition Time (TR) | 3,000–4,000 ms | Longer TR required for T2 contrast. |
| Inversion Time (TI) | 150–180 ms (for STIR) | Nulls fat signal at 1.5T for robust suppression. |
| Field-of-View (FOV) | 180 × 180 mm | Small FOV for high resolution of the perianal region. |
| Matrix | 256 × 256 | High matrix provides detailed visualization of sphincter anatomy. |
| Foldover Direction (Phase) | Right-to-Left (RL) | Reduces bowel motion artifacts and phase wrap. |
| Number of Slices | 20–25 | Covers from levator ani to perineal skin. |
| Slice Thickness | 3–4 mm | Medium thickness balances resolution and SNR. |
| Slice Gap | 0.3–0.4 mm | Minimal gap (10% of thickness) ensures complete coverage. |
| NEX / Averages | 2 | Higher averages improve SNR for small structure visualization. |
| Turbo Factor / ETL | 15–18 | High turbo factor for faster scanning while maintaining T2 contrast. |
| Bandwidth | 150–200 Hz/px | Medium bandwidth balances chemical shift reduction with SNR. |
| Fat Suppression | STIR | More robust than SPAIR when field inhomogeneity is present. |
| Fold-over Suppression | Yes | Prevents wrap-around artifacts from pelvic structures. |
✅ Correct Planning:

Planning Instructions:
Parameters for Coronal T2 TSE Fat-Saturated:
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 90–110 ms | Longer TE required for T2 contrast to highlight fluid. |
| Repetition Time (TR) | 3,000–4,000 ms | Longer TR required for T2 contrast. |
| Inversion Time (TI) | 150–180 ms (for STIR) | Nulls fat signal at 1.5T for robust suppression. |
| Field-of-View (FOV) | 200 × 200 mm | Wide enough to include bilateral ischiorectal fossae. |
| Matrix | 256 × 256 | High matrix for detailed anatomical visualization. |
| Foldover Direction (Phase) | Right-to-Left (RL) | Reduces motion artifacts from bowel and breathing. |
| Number of Slices | 15–20 | Covers from posterior rectum to anterior pubis. |
| Slice Thickness | 3–4 mm | Medium thickness balances resolution and SNR. |
| Slice Gap | 0.3–0.4 mm | Minimal gap (10% of thickness) ensures complete coverage. |
| NEX / Averages | 2 | Higher averages improve SNR for pathology detection. |
| Turbo Factor / ETL | 15–18 | High turbo factor for efficient T2 contrast acquisition. |
| Bandwidth | 150–200 Hz/px | Medium bandwidth reduces chemical shift while preserving SNR. |
| Fat Suppression | STIR | Robust suppression despite field inhomogeneity from gas. |
| Fold-over Suppression | Yes | Prevents aliasing from lateral pelvic structures. |
✅ Correct Planning:
Planning Instructions:
Parameters for Sagittal T1 TSE (Pre-contrast):
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 10–15 ms | Short TE required for T1 contrast. |
| Repetition Time (TR) | 400–600 ms | Short TR required for T1 contrast. |
| Field-of-View (FOV) | 200 × 200 mm | Matches T2 sequences for comparison. |
| Matrix | 256 × 256 | Medium-high matrix for good anatomical detail. |
| Foldover Direction (Phase) | Foot-to-Head (FH) | Consistent with other sagittal sequences. |
| Number of Slices | 15–20 | Matches coverage of T2 sequences. |
| Slice Thickness | 3 mm | Thin slices for detailed anatomy. |
| Slice Gap | 0.3 mm | Minimal gap (10% of thickness) for continuity. |
| NEX / Averages | 1–2 | Standard averaging for T1 contrast. |
| Turbo Factor / ETL | 3–5 | Low turbo factor preserves T1 contrast. |
| Bandwidth | 150–200 Hz/px | Medium bandwidth for balanced SNR and artifact reduction. |
| Fold-over Suppression | Yes | Prevents wrap artifacts. |
| Parallel Imaging | Optional (GRAPPA 2) | Reduces scan time if multi-channel coil available. |
After administering gadolinium contrast (typically 0.1 mmol/kg body weight), wait approximately 30-60 seconds before acquiring post-contrast images.
✅ Correct Planning:
Planning Instructions:
Parameters for Sagittal T1 TSE Post-contrast:
| Parameter | Recommended Values | Why These Values |
|---|---|---|
| Echo Time (TE) | 10–15 ms | Short TE required for T1 contrast. |
| Repetition Time (TR) | 400–600 ms | Short TR required for T1 contrast. |
| Field-of-View (FOV) | 200 × 200 mm | Matches pre-contrast for direct comparison. |
| Matrix | 256 × 256 | Medium-high matrix for good anatomical detail. |
| Foldover Direction (Phase) | Foot-to-Head (FH) | Consistent with pre-contrast sequence. |
| Number of Slices | 15–20 | Matches pre-contrast coverage exactly. |
| Slice Thickness | 3 mm | Same as pre-contrast for comparison. |
| Slice Gap | 0.3 mm | Minimal gap (10% of thickness) for continuity. |
| NEX / Averages | 1–2 | Standard averaging for T1 contrast. |
| Turbo Factor / ETL | 3–5 | Low turbo factor preserves T1 contrast. |
| Bandwidth | 150–200 Hz/px | Medium bandwidth for balanced SNR and artifact reduction. |
| Fat Suppression | Optional (Spectral) | Improves visualization of enhancing tissue by suppressing fat. |
| Fold-over Suppression | Yes | Prevents wrap artifacts. |
| Parallel Imaging | Optional (GRAPPA 2) | Reduces scan time if multi-channel coil available. |
The table below lists the 5 common anal fistula artifacts, and what techniques you can use to avoid them:
| Artifacts | Solution – How to Avoid It |
|---|---|
| Motion artifacts | Shorten scan time using parallel imaging or radial k-space acquisition (BLADE/PROPELLER). |
| Susceptibility artifacts | Use turbo spin echo instead of gradient echo sequences to reduce sensitivity to gas interfaces. |
| Wrap-around artifacts | Activate fold-over suppression to prevent anatomy outside the field of view from overlapping. |
| Chemical shift artifacts | Increase the bandwidth to reduce the spatial displacement between fat and water signals. |
| Fat suppression failure | Use STIR instead of spectral fat saturation when field inhomogeneity is present. |
Finally, we will review the images to ensure all the anatomical information we need is clear.
These key structures must be clearly visible in an anal fistula MRI:
Below, we will go through all the different image contrasts and explain their specific role in imaging anal fistulas.
T2-weighted imaging makes fluids appear bright. This contrast is ideal for tissues and abnormalities with high water content.
In anal fistula MRI, T2 sequences are the workhorse for detecting fistula tracts, which appear as bright tubular structures against darker muscle and fat. They help us map the exact course of fistulas through the sphincter complex and identify branching patterns.
We acquire sagittal views to assess the relationship between fistulas and the rectum, and to understand anterior-posterior spread.
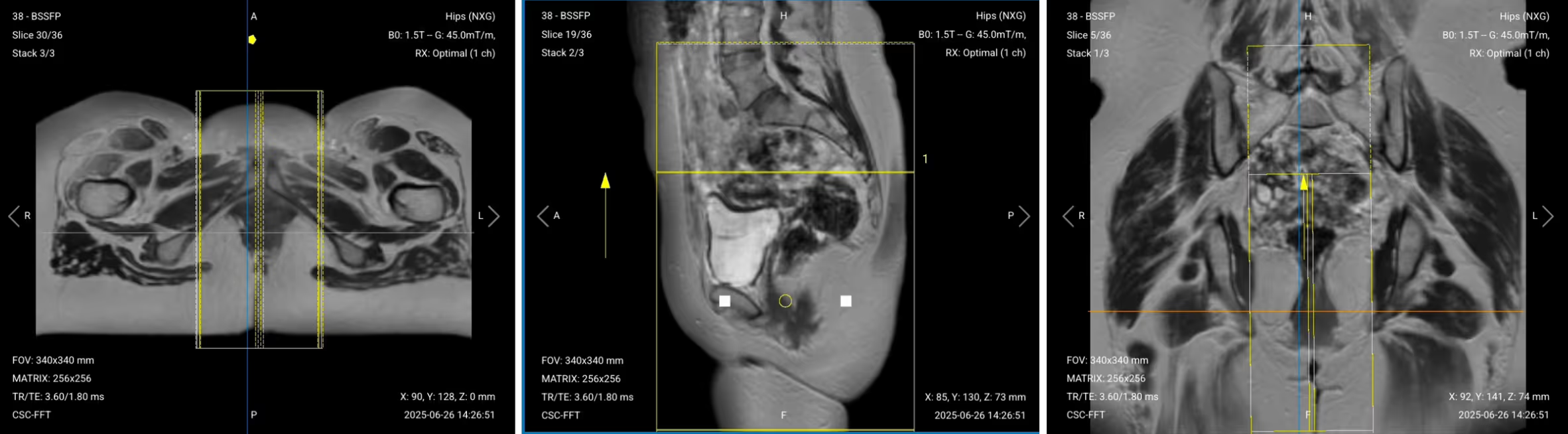
✅ Sagittal T2 TSE of Anal Canal – Correct Image Example:

Things to Look for in Sagittal T2 TSE:
T2 Fat-Saturated imaging suppresses fat while keeping fluid bright. This shows all areas with increased water content, making it the most sensitive sequence for detecting inflammatory spread.
In anal fistula MRI, STIR reveals the full extent of inflammation by highlighting edema in tissues. Any area with increased water appears bright, whether from acute infection or chronic inflammation. This complete map of inflammatory spread helps surgeons plan their approach.
We acquire fat-saturated T2 in all three planes to fully understand the fistula's path and extent:
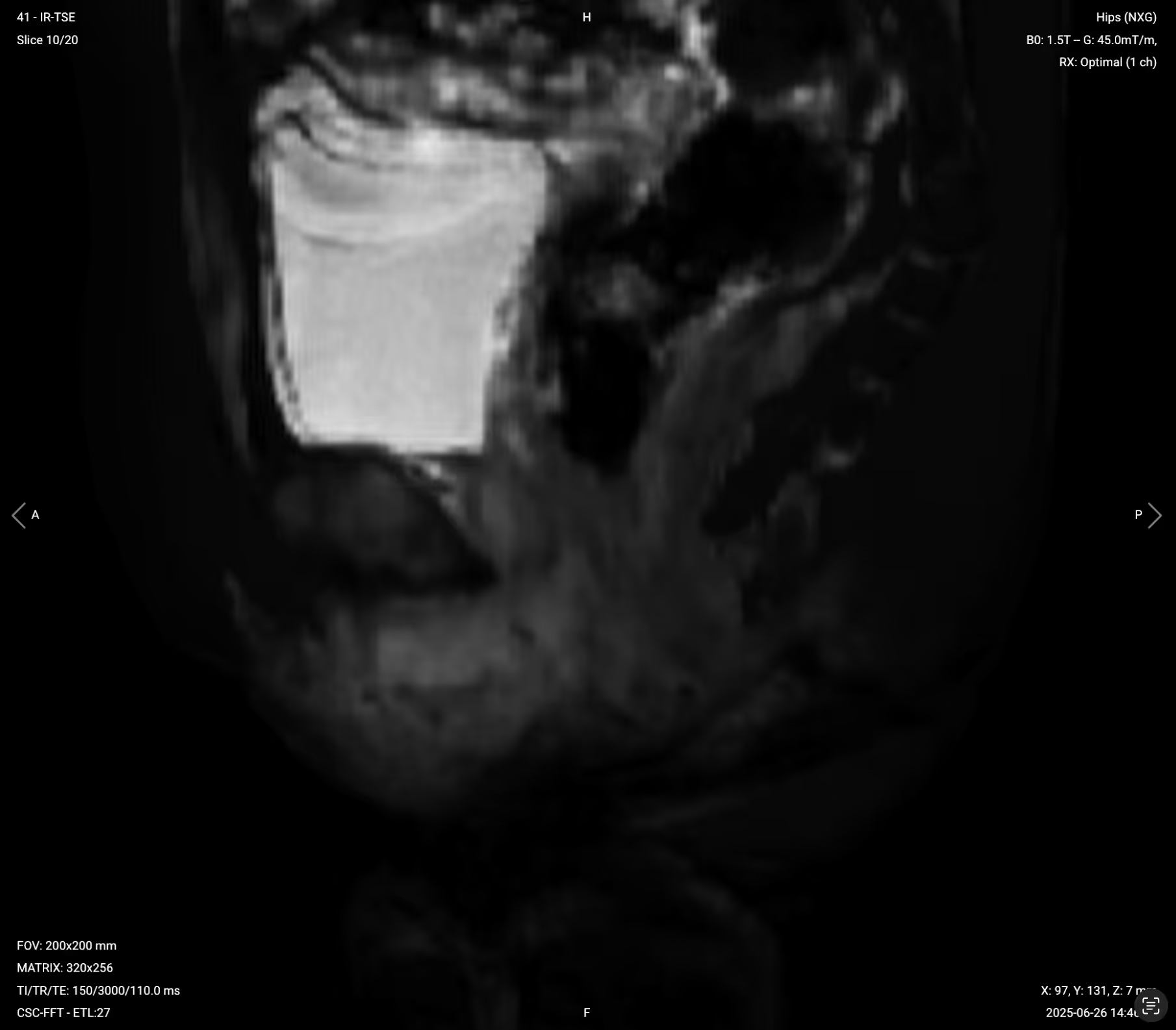
❌ Failed Spectral Fat Saturation (SPAIR) – Example of Poor Suppression:
%20Fat%20Saturation%2C%20Failed.avif)
Signs of Failed Fat Suppression:
✅ Sagittal T2 STIR of Anal Canal – Correct Image Example:
Things to Look for in Sagittal T2 Fat-Saturated:
We then acquire axial views perpendicular to the anal canal for the most diagnostic images, as they show tracts crossing from internal to external sphincter clearly.
✅ Axial T2 STIR of Anal Canal – Correct Image Example:

Things to Look for in Axial T2 Fat-Saturated:
✅ Coronal T2 STIR of Anal Canal – Correct Image Example:

Things to Look for in Coronal T2 Fat-Saturated:
T1-weighted imaging makes fat appear bright and fluid dark. This contrast is ideal for fat-rich tissues and structural abnormalities. T1 shows anatomical structures clearly, since it helps us see where different solid tissues like muscle and fat meet.
In anal fistula MRI, pre-contrast T1 sequences provide baseline anatomy and help identify chronic fibrotic changes. They show the normal fat planes between muscles and help detect fat infiltration or obliteration that indicates chronic inflammation.
We acquire pre-contrast T1 in the sagittal plane to match our T2 sequences for direct comparison.
✅ Sagittal T1 TSE Pre-contrast of Anal Canal – Correct Image Example:

Things to Look for in Sagittal T1 Pre-contrast:
Post-contrast T1 shows where gadolinium accumulates in tissues with active blood supply and leaky vessels. Enhancement indicates viable, vascularized tissue.
In anal fistula MRI, post-contrast T1 differentiates healing tissue from mature scar. Active granulation tissue in fistula walls enhances brightly, while chronic fibrotic tracts show little to no enhancement. Abscesses show characteristic rim enhancement around a dark center of pus.
These contrasts help surgeons identify which tissue can heal versus what needs removal.
We typically acquire post-contrast T1 in the same sagittal plane as pre-contrast for direct comparison. Some protocols may add axial or coronal post-contrast sequences for complex cases.
✅ Sagittal T1 TSE Post-contrast of Anal Canal – Correct Image Example:

Things to Look for in Sagittal T1 Post-contrast:
Before finishing an anal fistula MRI, always check these 5 points to ensure diagnostic quality: